Overdiagnosis of Cancer, Defined
/Researchers from Dartmouth are pitching a standard definition for "overdiagnosis" in cancer screening. Will it hold up?
Read MoreWe Should Be Transplanting More Organs from Individuals Who Died of Drug Overdose
/Organs from donors who died from overdose are "discarded" more than from other donors. That might not be the right choice.
Read MoreNew Drugs Hold Real Promise for Metastatic Melanoma
/I'm going to show you a survival curve for metastatic melanoma.
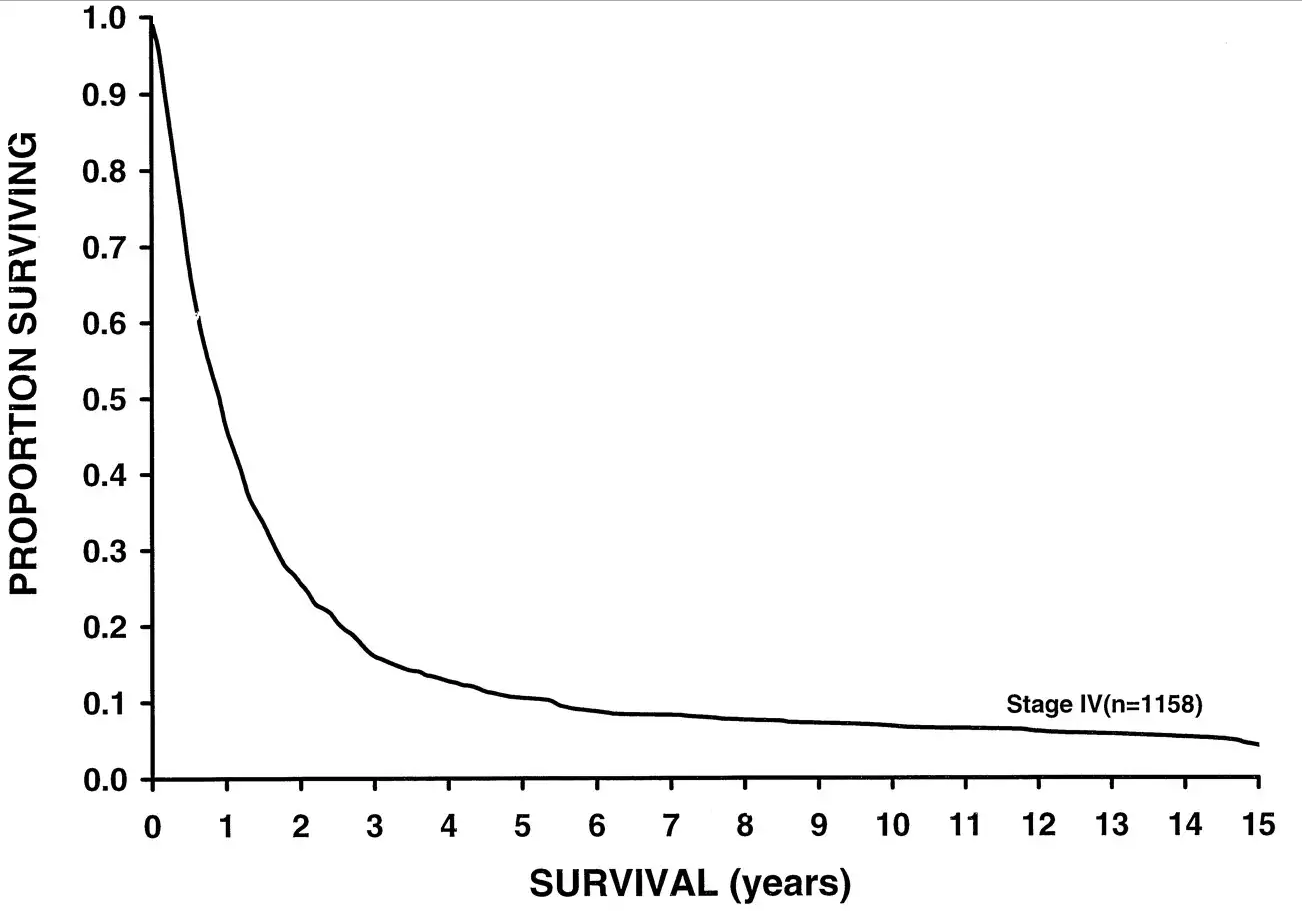
This data was analyzed in 2001, but sadly, even current 5 year-survival for metastatic melanoma sits around 15%. But some new drugs might change this.
For the video version of this post, click here.
Here's a chart examining Melanoma-associated mortality rates over time:
Compare that to breast cancer, which has seen some dramatic therapeutic advances over the past few decades:
But melanoma is riding a wave of novel immunotherapies that hold promise to change the treatment landscape substantially.
Appearing in the Journal of the American Medical Association is a type of study we don't see too much of these days. It's not really a clinical trial. It's not really a meta-analysis. Frankly, I'm not sure what to call it – an aggregate analysis perhaps?
The study examines 655 patients treated with the PD-1 inhibitor pembrolizumab from 2011 to 2013. Yup, that's the same pembrolizumab which was used so successfully to treat this charming former president:
A brief aside here. Pembrolizumab is a monoclonal antibody directed towards programmed cell death protein 1, PD-1. PD-1 acts to prevent immune cells from attacking your own cells – it's an immune "checkpoint" making pembrolizumab one in a class of "checkpoint inhibitors". Basically, by blocking PD-1, pembrolizumab allows your immune system to attack your own cells. Not something you want under ordinary circumstances, but perhaps beneficial when your own cells have turned against you.
Merck has bet big on pembrolizumab, with clinical trials ongoing or planned in melanoma, non-small-cell lung cancer, small-cell lung cancer, ovarian cancer, glioma, colorectal cancer, and on and on. What happens when a company is doing so many trials like this is a kind of fractionation, where you lose the aggregate knowledge of patient experiences because they are spread out across so many trials.
So I was gratified to see this aggregate analysis which examined patients with advanced melanoma receiving pembrolizumab across four different trials. See, if you do four trials, and one is nice and positive, and the others are equivocal, and you are a for-profit drug company, maybe you're more likely to try to get that positive trial into some high-profile journal, and let the others either languish in peer-review hell or get published in an out-of-the-way rag.
What we get in JAMA, though, is a study with adequate power to demonstrate that pembrolizumab might make a difference.
Among all the patients treated with pembrolizumab (and yes, there is no control group reported here), the objective response rate was 33%. The median overall survival was 23 months, and 31 months among those for whom pembrolizumab was the first systemic cancer therapy. Compared to the historical median survival of under a year, this represents a substantial improvement.
Interestingly, among those who responded to the drug initially, the duration of response was fairly long. In fact, at 2 years, around 70% of people who initially responded to the drug were still responding. This is a good thing, as it demonstrates that development of resistance to therapy might be limited.
Now, before we bestow too many accolades on Merck for giving us this aggregate data, we might ask whether they would have been as forthcoming if the trials weren't quite as successful. But, placing cynicism aside for the moment, it seems that this drug, or one of its competitors will have a place at the table in the treatment of advanced melanoma.
Competing risk: #2 on my list of most misinterpreted epidemiology concepts
/Competing risk is a tough concept. I think the reason people have so much trouble with it is that it sounds intuitive. When you hear "competing risk" you have this immediate sense that you know what it means. But in practice, competing risk works quite a bit differently from what you might expect. In a post written for MedPage today, I outlined the issues in interpretation of competing risk using my foray into nightlife as an analogy.
Check out the full post here.
Is there anything coffee can't do?
/For the video version of this post, click here.
Coffee. Its hard not to be biased when it comes to the ubiquitous drink. Many of us, myself included, depend on the stuff to start our day, continue our day, and give us something to do when we should otherwise be working. Studies linking coffee to better health get a lot of press. A few months ago, a big splash was made when a study linked coffee consumption to lower risk of melanoma (though they failed to account for sun exposure). Now, we have coffee staving off colon cancer.
The paper, appearing in the Journal of Clinical Oncology, examined roughly 1000 individuals with stage 3 colon cancer, who had been through at least the first round of surgery and chemotherapy. Each of them filled out a detailed food-frequency questionnaire within a couple months after the initial treatment, and they were followed prospectively for cancer recurrence or death.
The majority of the cohort reported drinking 1-3 cups of coffee per day. A small number, 6%, reported taking more than 4 cups per day. Heavy coffee drinkers were more likely to be male, white, and smokers, and had a higher level of physical activity.
After around 7 years of follow-up, 35% of the patients had experienced cancer recurrence or died. Among those who drank 4 or more cups of caffeinated coffee per day, the overall risk of recurrence or death was reduced by about 50% after adjustment for confounders.
Let that sink in a minute. 50%. Has one of the most potent anti-cancer agents been literally sitting under our nose all these years? Well, as much as Im a java fan, I might need to cool this off a bit.
First off, these patients were part of a clinical trial evaluating the role of adding irinotecan to standard adjuvant chemotherapy for colon cancer. Clinical trials recruit very specific patients - these results may not hold for your typical colon cancer survivor.
Another issue: Food frequency questionnaires generate a ton of data - you can't possibly control for everything people eat. The authors adjusted their results for total caloric consumption, but it is possible that foods that correlate with coffee intake are the actual drivers of the relationship here. Put simply, it's just as likely that this is a biscotti effect as a coffee effect.
Finally, the big issue: What do we mean when we say coffee? Is an espresso the same as a venti caramel macchiato? Does it matter where the beans come from? How they are roasted? How much sugar you add to it? This is the central problem of dietary research, and one that can only be overcome by randomized trials.
So lets do it. There seems to be enough data now to justify actually trying this under controlled settings. My prediction is that we wont see a 50% reduction in recurrence of colon cancer, but we may see something. After all, coffee is a drug. A wonderful, tasty, necessary drug that goes great with pie.










