Low Vitamin D Levels At Birth Linked to Schizophrenia in Adulthood
/A Danish study found that low vitamin D levels at birth were more common among those who eventually developed schizophrenia.
This week – a study appearing in Nature Scientific Reports strongly suggests a link between Vitamin D levels at birth, and the subsequent risk of schizophrenia.
European countries with their decades-long data collection on the entire population make great settings for epidemiologic research as well as dystopian science fiction novels.
Since 1981, Denmark has been collecting dried blood spots on all newborns in the country. These biosamples, frozen in time, were then linked to adult patients who had developed schizophrenia. The simple question – would Vitamin D levels at birth be related to schizophrenia later in life.
It’s not totally crazy. The same group had shown in an earlier study that abnormal Vitamin D levels at birth – either too low or too high – were associated with subsequent schizophrenia.
This larger study attempted to reproduce those findings.
In any case, they identified 1,301 individuals with schizophrenia and an equal number of age- and sex-matched controls. They then rehydrated those old dried blood spots and measured Vitamin D levels.
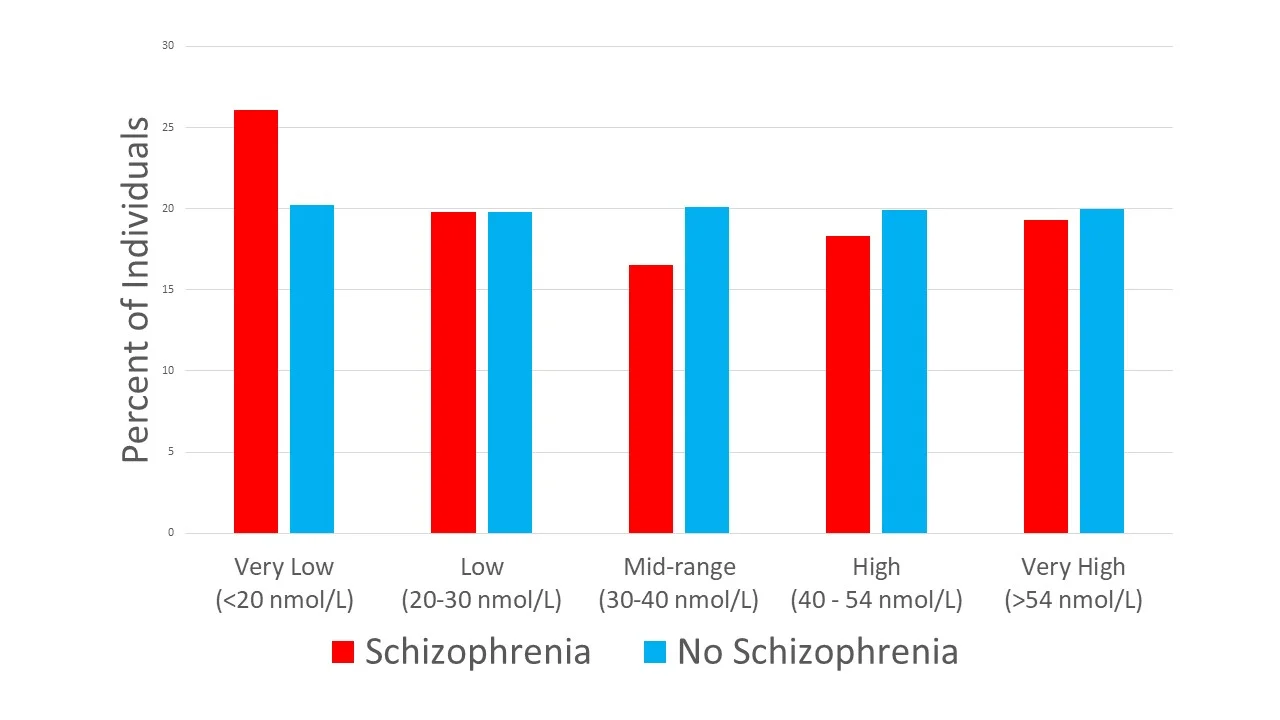
Really the only picture you need for this one.
The figure tells the main story – 26% of the individuals with schizophrenia were born with very low Vitamin D levels, only 20% of the controls were.
Even after adjustment for family history of mental illness, age, sex, urbanization at birth, maternal and paternal age, gestational age and birth weight, the finding persisted – low vitamin D: more schizophrenia.
Is vitamin D to schizophrenia what folic acid is to neural tube defects? The authors suggest as much, writing:
OK - No.
Let’s have some perspective. Folate supplementation decreased the rate of neural tube defects by 72% in a large, randomized study.
By the authors own calculation, only 8% of cases of schizophrenia can be attributed to low neonatal Vitamin D levels, even assuming low Vitamin D is causal.
Most neural tube defects are due to folate deficiency. Not so for Vitamin D and schizophrenia.
And, that’s the elephant in the room. Is it causal?
Remember, Vitamin D is the lifestyle biomarker. Higher levels are associated with all sorts of healthy behaviors, like being active, getting outside, eating a varied diet. Because of that, observational studies have suggested that Vitamin D might protect against colon cancer, dementia, heart disease, and virtually any other ill you can think of.
But here’s the catch. Interventional studies, where individuals are actually randomized to Vitamin D supplementation have almost all been underwhelming.
That suggests that much of the signal we see in studies like this are not due to Vitamin D per se, but the things that vitamin D levels stand in for. The authors have called for a randomized trial to figure out the Vitamin D – Schizophrenia link once and for all. These data support such a trial. But let’s not get our hopes too high. Not to be a downer, I’m just, you know, reality testing.
This commentary first appeared on medscape.com