Opioids Tie Non-opioid Painkillers in Randomized Trial, Which Means Opioids Lose.
/The JAMA study suggests that opioids may have little role in the treatment of chronic, non-cancer pain.
When two treatment modalities are being compared, I can usually find something positive to say about both of them.
But today we have this study, appearing in the Journal of the American Medical Association, comparing opioid to non-opioid regimens for chronic back or knee pain and I am hard-pressed to find a single data point that argues FOR the use of opioids in this setting.
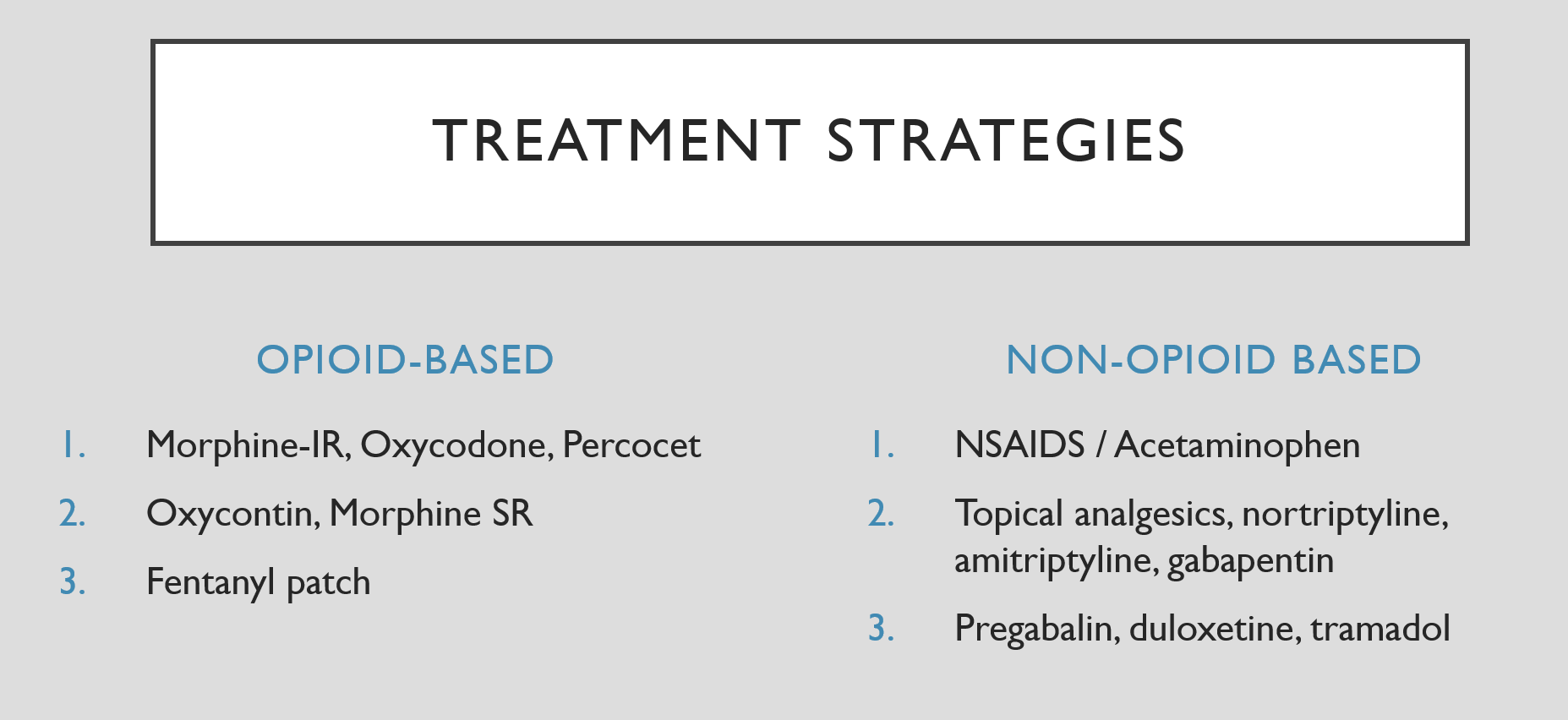
240 Veterans Affairs patients with moderate to severe chronic knee or back pain were randomized to one of the two treatment strategies, each of which had three tiers. Take a look:
The opioid group first tier was characterized by short-acting pain killers, then escalated to longer acting agents, and finally capped out with transdermal fentanyl.
The non-opioid regimen was a bit more clever, in my opinion. Tier 1 was acetaminophen and NSAIDs. Providers could then escalate to other oral meds (I particularly like the underused amitriptyline appearing in this tier) and topicals, and finally capped out with tramadol.
Now, I know what you're thinking. Isn't tramadol an opioid? I asked lead author Dr. Erin Krebs that very question. She reminded me that this trial started in 2010:
“This was before all the concerns about opioid overdose and addiction and back then a big concern was is it ethical to deprive patients of opioids if they fail all these non-opioid medications”.
Times have certainly changed. But regardless, only 13 patients in the non-opioid group ever required escalation all the way to tramadol.
And the results did not look good for opioids. The primary outcome was pain-related function which improved substantially in both groups but did not differ between the groups. Raw pain scores ended up being a bit better in the non-opioid arm.
Adverse events, as you might expect, were significantly higher in the opioid group, but fortunately no opioid abuse was detected.
One common criticism you hear about opioid trials is that researchers simply didn’t give enough – if they had titrated up more aggressively, patients would have better pain control. While the investigators limited the total morphine equivalents to 100 mg per day, Dr. Krebs told me very few patients bumped into that ceiling.
“The vast majority of folks stopped before 50, and it wasn’t because we had a limit there. It’s because simply that seemed to be the best dose for them”.
Are opioids dead for chronic back or knee pain? I think they are on life support. But the real key to this study was the careful titration of non-opioid pain medication in that group. Most of us try Tylenol and Advil and then give up. With close monitoring, patient feedback, and a willingness to try multiple interconnected agents including tricylclics, physicians may find that treating chronic pain is not so painful after all.