Are Physicians Responsible for the Opioid Epidemic?
/For the video version, click here.
When I see a patient in clinic, I’m given a sheet with their vital signs like this.
Blood pressure: 142/65. Heart rate 74. Pain: 5 out of 10. I’m a nephrologist. I specialize in chronic kidney disease – a completely painless condition. But there has been a coordinated and I think well-intentioned campaign to increase physicians’ awareness of patient pain. Some have argued that the adoption of pain as the “fifth vital sign” has led to an increased rate of opioid prescription, addiction, and overdose.
It is quite clear that overdose deaths are increasing.
In the face of data like this, we are forced to examine our own responsibility as physicians. Do these numbers reflect some deeper societal issues, or is our prescribing behavior to blame?
The hypothesis is that a patient gets an initial opioid prescription, and, due to the well-documented addictive properties of opioids, turns into a chronic abuser of the drugs.
This article appearing in the journal Pain attempts to quantify just how frequently this pathway is followed.
The researchers used MarketScan data – this is a huge database of mostly employer-insured individuals – and identified a bit over 10 million individuals with a new opioid prescription between 2003 and 2013. These were matched with controls who never got an opioid prescription.
Those who got opioids were more likely to have an antecedent history of opioid use disorder, substance use disorder, and a host of other psychiatric problems. They were also significantly more likely to have received psychotropic medications.
So opioid prescriptions are going to some high-risk individuals. But how many of those would turn into chronic users?
The study concludes – not that many. After 18 months, only 1.3% of individuals had transitioned from one-time to chronic use… at least based on prescription records.
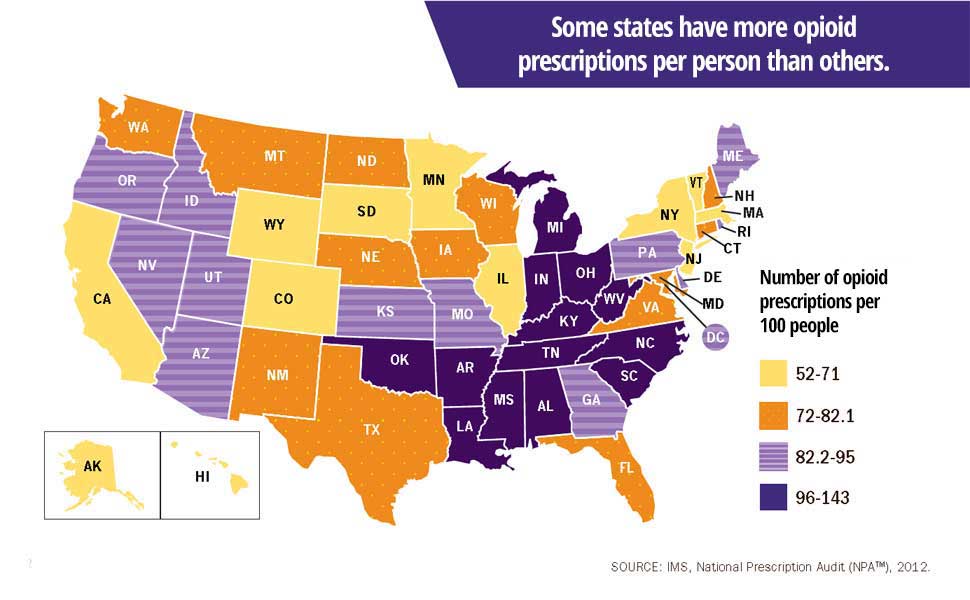
How do we think about that 1.3%? It may seem like a small percentage that isn’t worth worrying about, but multiply that by the number of prescriptions we’re handing out per year: about one for every person in the country.
And also realize that that 1.3% is an underestimate.
MarketScan largely captures people who are productively employed, and it’s only capturing chronic prescription opioids. Most opioid abuse comes from sources other than the individuals doctor:
This chart shows that most non-medical users of prescription opioids get them from friends or family, not their doctor.
And this study, appearing in JAMA in 2008 found that diverted drugs were the major source of opioid overdoses:
We need to update our conceptual model to look like this:
The major unknown here is the rate of transition from licit to illicit opioid use. And that data is harder to find than, well, street fentanyl nowadays. We also need to know the REASON for that initial opioid prescription. It is a VERY different thing to receive oxycodone after you have your wisdom teeth removed and to receive it for chronic low back pain, and the risk of transition to opioid use disorder is much higher in the latter.
In 2016, the CDC came down hard on opioid prescriptions for CHRONIC conditions. This is the correct framework. Are docs responsible for the rise in opioid abuse and deaths in this country? Not exclusively. But we can’t deny that somewhere in the chain of events that leads to opioid abuse lies a prescription pad.