Contrast Nephropathy: The Biggest Cause of Acute Kidney Injury that Might Not Exist
/For the video version, click here.
We just had a patient in the hospital with respiratory failure. A bedside echo revealed right heart strain, so there was a concern for pulmonary embolism. A CT scan with contrast would rule in or out the diagnosis. But the patient’s creatinine was 2.5. A debate ensued. Should we do the definitive study or the less-definitive V/Q scan to avoid the risk of acute kidney injury from IV contrast?
For decades, iodinated contrast material has been implicated as a major contributor to AKI. It was sort of a given. But there has always been a voice of dissent in that area of research. There's never been a real randomized trial. And people who get contrast may be sicker than those who don't need contrast. Beyond that, older contrast agents were hyperosmolar. Newer contrast agents are not.
Now a growing body of papers, including this one appearing in the Annals of Emergency Medicine, have brought contrast’s role in the development of AKI into question.
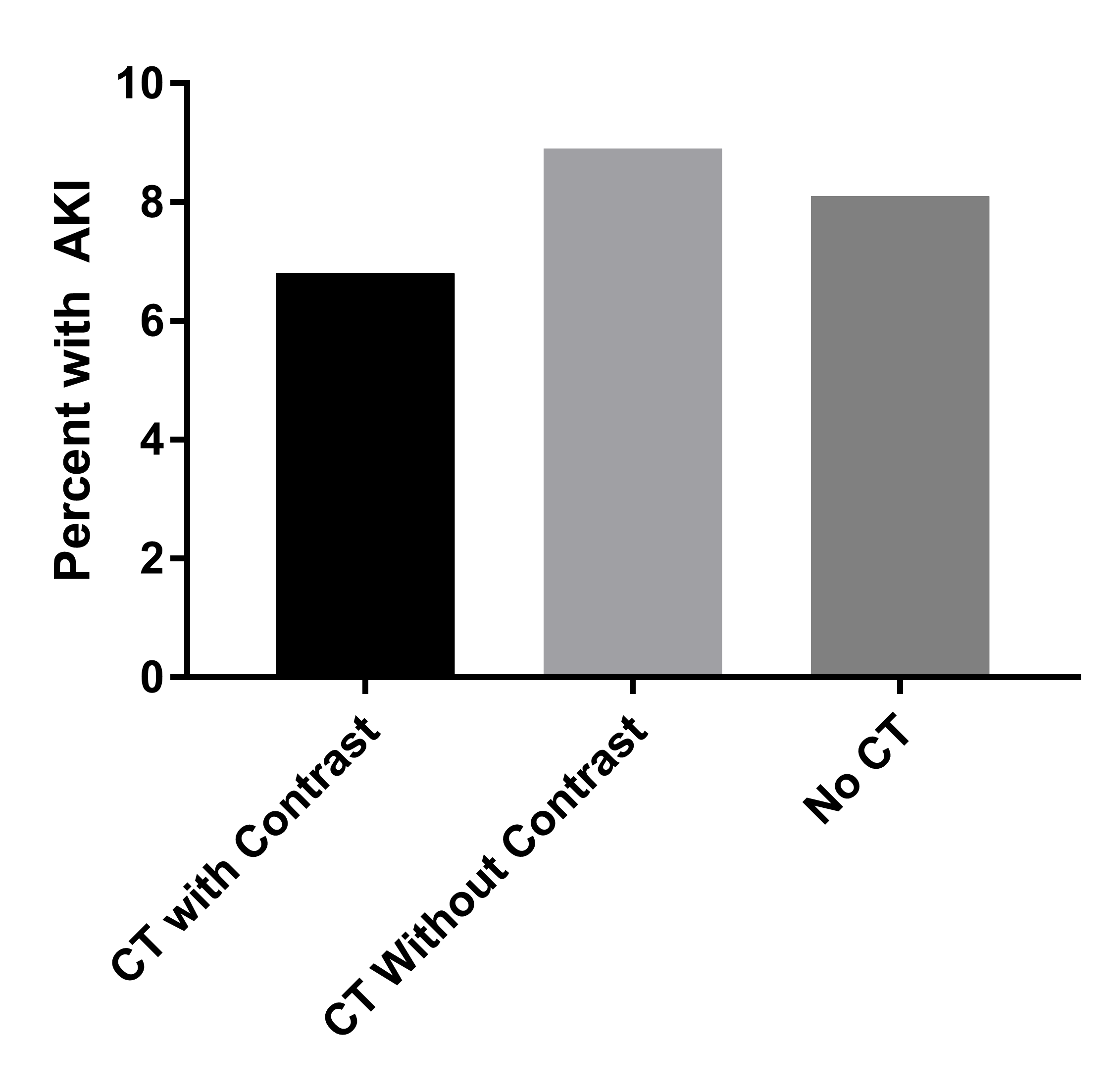
This was a single-center study that examined 16,801 patients who were seen in the Emergency Department and had two creatinine values measured at least 48 hours apart. About 40% of them got a CT scan with contrast, 30% a CT without contrast, and 30% got no CT scan at all. The researchers then looked at the rates of AKI in those three groups.
Rates of AKI ranged from 7 – 9%. The highest frequency was in the non-contrast group, followed by the group that got no CT scan at all, then those who got a CT with contrast. Does this prove that contrast is actually protective?
Of course not. This is a classic case of selection bias. Physicians are more likely to give contrast if they feel the patient is at low risk of AKI, so we see a lower risk in that group.
The authors tried to adjust for this using something called propensity score matching which is a statistical technique that attempts to minimize this type of bias.
After propensity score matching, the authors found no evidence that contrast lead to AKI. Across any subgroups, even among those with poor kidney function.
Case closed? Not exactly. Propensity score matching isn't perfect. There may still be factors that are pushing clinicians to avoid contrast in certain patients that weren’t measured. This would tend to make contrast look safer than it is.
The propensity score also included chronic comorbidities. These were extracted based on ICD-9 codes, but these codes can be entered at any time of the hospital admission, even after AKI developed. Using future information in a propensity score can seriously bias the results either for or against contrast and violates one of the ten commandments of statistics.
As a nephrologist, I still suspect there is some risk to iodinated contrast, though it's probably a bit overblown. One thing is for sure though. The evolution of research in this area is truly a study in contrasts.