A First-In-Class Oral Pain Medication May Change the Game
/VX-548 (brand name to be determined) may provide acute pain control without the risks associated with other drugs.
When you stub your toe, or get a paper cut on your finger, you feel the pain in that part of your body. It feels like the pain is coming from that place. But of course, that’s not really what is happening. Pain doesn’t really happen in your toe or your finger. It happens in your brain.
It’s a game of telephone, really. The afferent nerve fiber detects the noxious stimulus, passing that signal to the 2nd order neuron in the dorsal root ganglia of the spinal cord, which runs it up to the thalamus to be passed to the 3rd order neuron which brings it to the cortex for localization and conscious perception. It’s not even a very good game of telephone. It takes about 100ms for a pain signal to get from the hand to the brain – longer from the feet given the greater distance. You see your foot hit the corner of the coffee table and have just enough time to think “oh no” before the pain hits.
Source: Bettina Guebeli, CC BY-SA 4.0 <https://creativecommons.org/licenses/by-sa/4.0>, via Wikimedia Commons
Given the Rube-Goldberg nature of the process, it would seem like there are any number of places we could stop pain sensation. And sure, local anesthetics at the site of injury, or even spinal anesthetics are powerful – if temporary and hard to administer – solutions to acute pain.
But in our everyday armamentarium, let’s be honest we essentially have three options. Opioids, which activate the mu-receptors in the brain to dull pain (and cause a host of other nasty side effects), NSAIDs, which block prostaglandin synthesis and thus limit the ability for pain-conducting neurons to get excited, and acetaminophen which, despite being used for a century, is poorly understood.
But this week, we enter the prologue of what might be the next big story in pain control. Let’s talk about VX-548.
If you were to zoom in on the connection between that first afferent pain fiber and the secondary nerve in the spinal cord dorsal root ganglion, you would see a receptor called Nav1.8 - a voltage-gated sodium channel.
This receptor is a key part of the apparatus that passes information from nerve-1 to nerve-2, but only for fibers that transmit pain signals. In fact, humans with mutations in this receptor that leave it always in the “open” state have a severe pain syndrome. Blocking the receptor, therefore, might reduce pain.
In pre-clinical work, researchers identified VX-548, which doesn’t have a brand name yet – as a potent blocker of that channel even in nanomolar concentrations. Importantly, the compound was highly selective for that particular channel, about 30,000 times more selective than it was for the other sodium channels in that family. ‘
Of course – a highly selective and specific drug does not a blockbuster analgesic make. To determine how this drug would work on humans in pain, they turned to two populations – 303 individuals undergoing abdominoplasty, and 274 undergoing bunionectomy as reported in a new paper in the New England Journal.
I know this seems a bit random, but abdominoplasty is quite painful and a good model for soft-tissue pain. Bunionectomy is also quite a painful procedure, and a useful model of bone pain.
After the surgeries, patients were randomized to several different doses of VX-548, hydrocodone + acetaminophen, or placebo for 48 hours.
Source: Jones et al, NEJM 2023
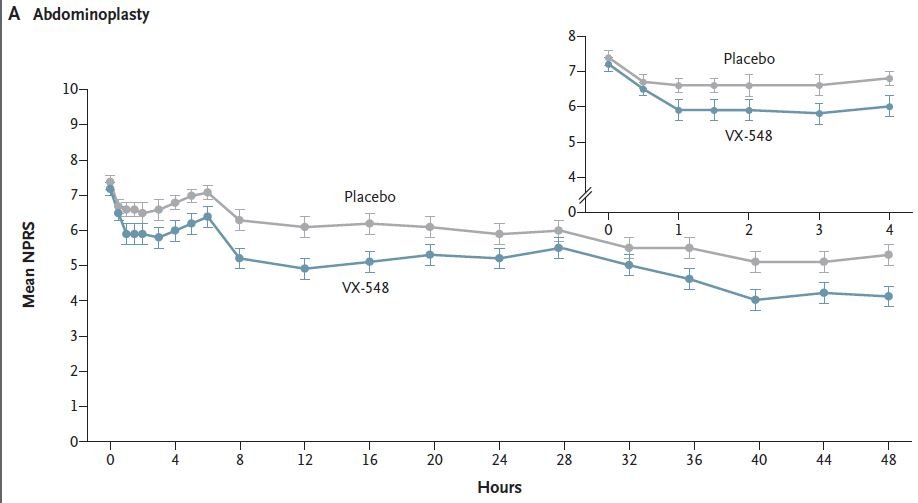
At 19 time points over that 48 hour period, participants were asked to rate their pain on a scale from 0 to 10. The primary outcome was the cumulative pain experienced over the 48 hours – so higher pain would be worse here, but longer duration of pain would also be worse.
And the story of the study is really told in this chart.
Source: Jones et al, NEJM 2023
Yes, those assigned to the highest dose of VX-548 had a statistically significant lower cumulative amount of pain in the 48 hours after surgery. But the picture is really worth more than the stats here. You can see that the onset of pain relief was fairly quick, and that pain relief was sustained over time. You can also see that this is not a miracle drug. Pain scores were a bit better 48 hours out, but only by about a point and a half.
Placebo isn’t really the fair comparison here – few of us treat our post-abdominoplasty patients with placebo, after all. The authors do not formally compare the effect of VX-548 to that of the opioid hydrocodone, for instance. But that doesn’t stop us.
This graph, which I put together from data in the paper, shows pain control across the four randomization categories, with higher numbers indicating more (cumulative) control. While all the active agents do a bit better than placebo, VX-548 at the higher dose appears to do the best. But I should note that 5mg of hydrocodone may not be an adequate dose for most people.
Yes, I would really have killed for an NSAID arm in this trial. Its absence, given that NSAIDs are a staple of post-operative care, is… well, let’s just say notable.
Although not a pain-destroying machine, VX-548 has some other things to recommend it. The receptor is really not found in the brain at all, which suggests that the drug should not have much risk of dependency, though that has not been formally studied.
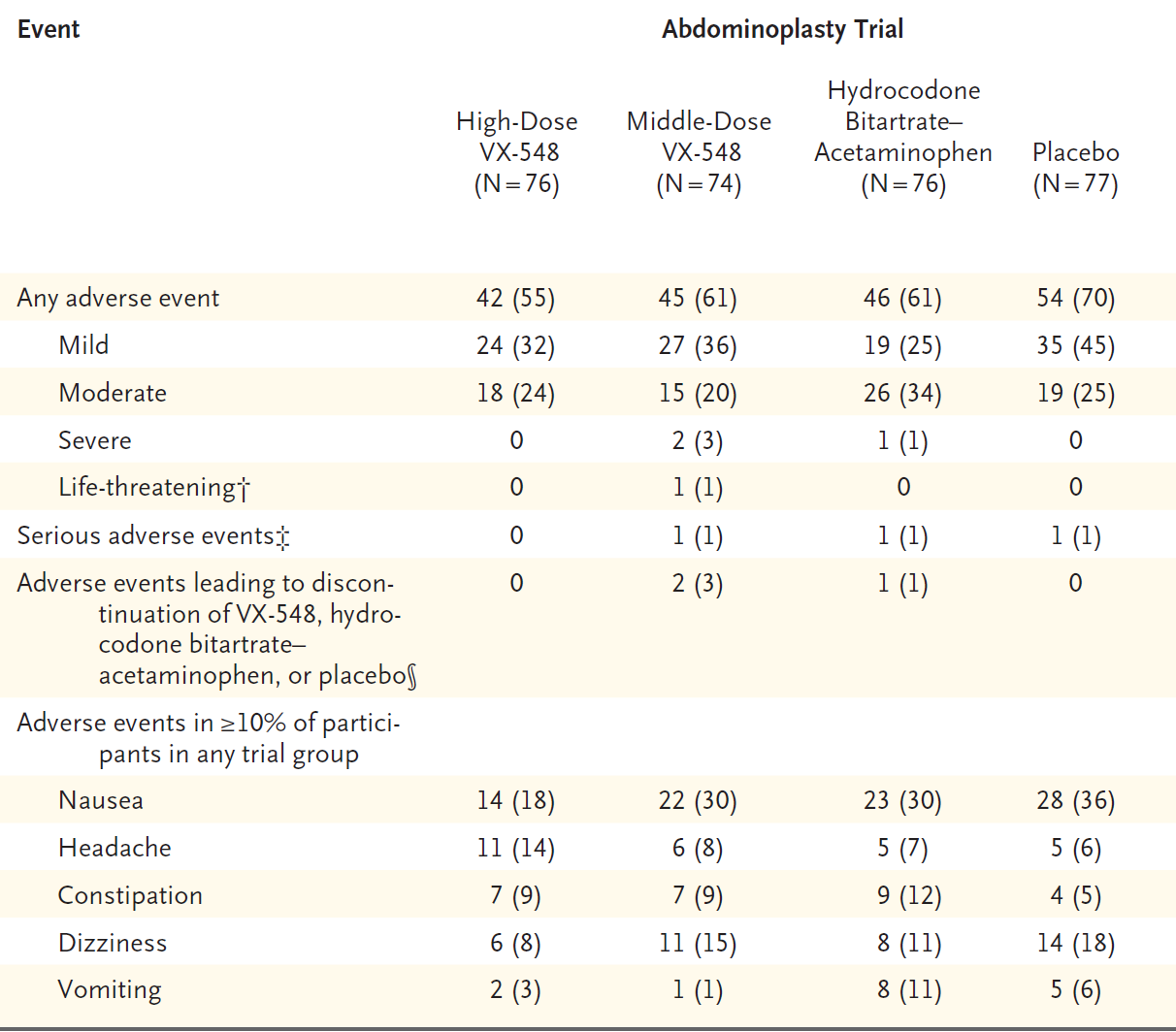
The side-effects were generally mild – headache was the most common – and less prevalent than what you see even in the placebo arm.
Source: NEJM 2023
Perhaps most notable, the rate of discontinuation of the study drug was lowest in the VX-548 arm. Patients could stop taking the pill they were assigned for any reason, ranging from perceived lack of efficacy to side-effects, and a low discontinuation rate indicates to me a sort of “voting with your feet” that suggests this might be a well-tolerated and reasonably effective drug.
VX-548 isn’t on the market yet – phase 3 trials are ongoing. But, whether it is this particular drug, or another in this class, I’m happy to see researchers trying to find new ways to target that most primeval form of suffering – pain.
A version of this commentary first appeared on Medscape.com.