New Data: Vitamin D Supplements Unlikely to Prevent COVID-19
/Mendelian randomization helps to tease out causality, and there does not seem to be a causal link between Vitamin D level and COVID-19.
This week – we’re going to dive into the lion’s den once again with this study, appearing in PLOS Medicine, failing to show a causal link between Vitamin D levels and COVID-19 incidence or severity.
And I know this is one of those hot button COVID issues – I think it’s because we all really want there to be a cheap, easy way to avoid getting COVID or getting severe COVID. And, technically, there is – it’s a vaccine – but sure it would be nice if there were something we had a lot more experience with – I get that.
And the observational data was definitely compelling. People with low Vitamin D levels really do have worse COVID outcomes. Much worse.
But correlation isn’t causation. You’ve heard that before, but we rarely dwell on what it really means. Why is causation so important? It’s because if A causes B, then changing A changes B. When we ask if low vitamin D levels cause worse COVID, what we are really saying is – if I boost Vitamin D levels can I protect against COVID.
If there is causation, the answer is yes. But there might not be. Lots of things reduce Vitamin D levels and increase the risk for COVID. I’ve often referred to Vitamin D level as the lifestyle biomarker – higher in healthy, active people – the very people who you’d expect would do pretty well if they got COVID.
The classic way to assess causality in medicine is via the randomized trial, and we have a few trials of Vitamin D supplementation in COVID out there now. I made a quick table to highlight what is known.
Vitamin D and COVID RCTs
Mixed results here from some pretty small studies, all of which focused on people who were already sick. The largest study says no benefit, smaller less well-controlled studies find some benefit in soft outcomes. None of them answer the question of whether providing Vitamin D supplementation to otherwise healthy people would affect COVID later on.
So – are we stuck?
It turns out there is a clever way to assess causality that doesn’t require a randomized trial. It’s not perfect, but it might be the best we have. It’s called Mendelian Randomization.
Here’s how it works.
We have a causality question – does low Vitamin D level cause worse COVID? But we know that the Vitamin D level is affected by a bunch of lifestyle and environmental factors that we can’t possibly control for. But something else affects your Vitamin D level – your genes.
Some people are genetically predisposed to have higher Vitamin D levels, just like some people are genetically predisposed to be taller. Sure, your actual vitamin D level will be affected by all that other stuff – but your genes don’t change.
If low vitamin D is causally linked to worse COVID, people with a genetic predisposition to low Vitamin D will have worse COVID than people with a genetic predisposition to have high Vitamin D. Those genes basically bypass all the noise of the real world. It’s a pretty neat trick honestly.
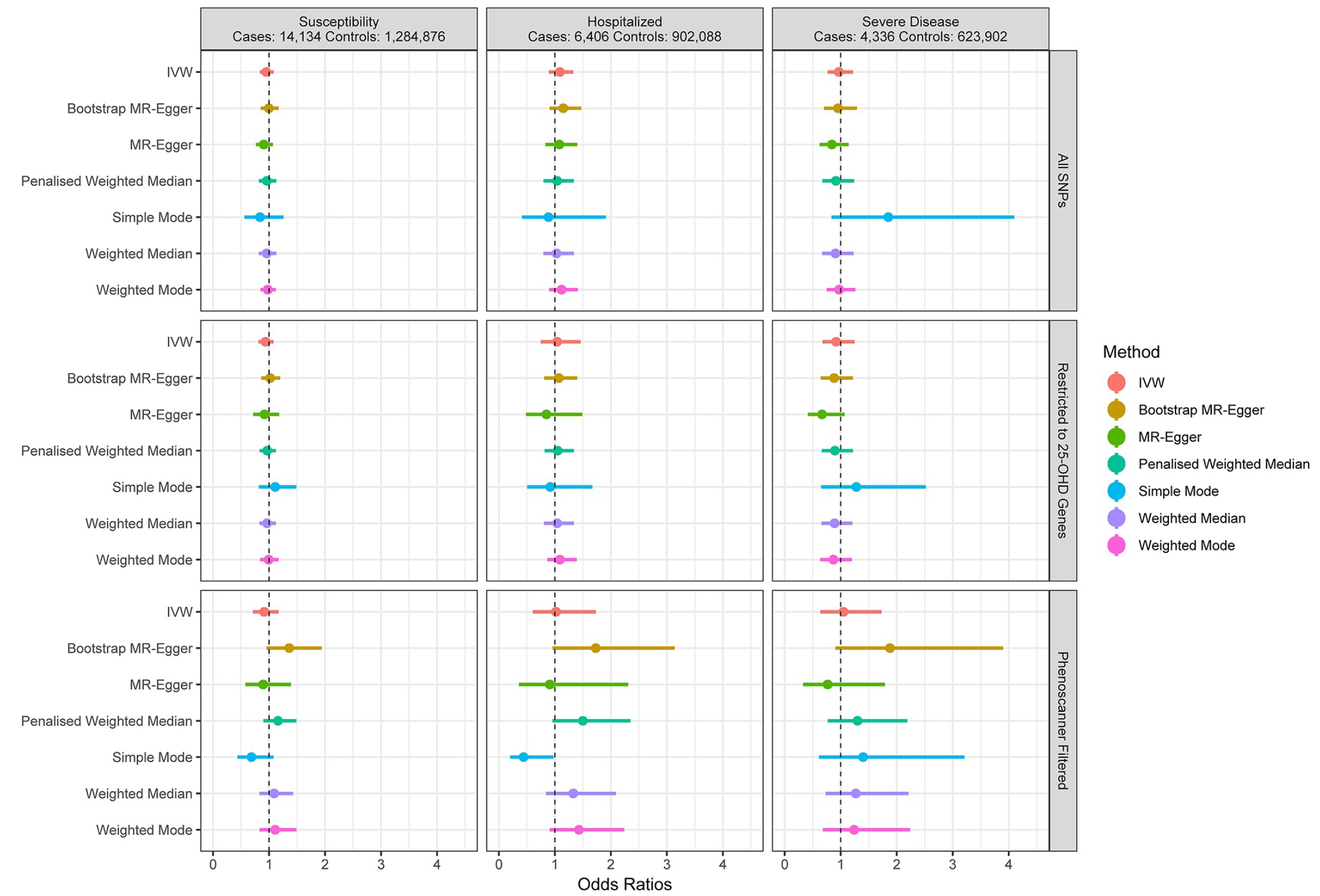
A bunch of ways to say “no signal”
Of course, you need a TON of data to figure out what genes (or in this case tiny pieces of genes called SNPs) lead to higher Vitamin D levels. Researchers in this study used about 450,000 people to create a genetic risk profile for low Vitamin D levels. They then used that score to assess the genomes of around 14,000 people with COVID and 1.3 million people without COVID. If low Vitamin D levels are causally linked to worse COVID, you’d expect the COVID group to be enriched for people with a genetic predisposition to have low Vitamin D.
But – this wasn’t seen. Not for susceptibility to COVID, not for hospitalization with COVID, not for severe disease. This figure basically says: we tried this a bunch of different ways and no matter what we don’t see a protective signal.
At this point, we have little support for Vitamin D supplementation as a preventative strategy.
A few caveats though. First, it’s important to remember that this analysis was not restricted to people who are Vitamin D deficient. Very low levels, of any vitamin really, should be repleted. I mean, that’s why they’re vitamins.
How we measure Vitamin D
There is also a subtler issue with these Mendelian randomization studies of vitamin D. You know that genetic risk score they are calculating? It is based on the measured Vitamin D level. But the vitamin D level we measure the blood is not the same as the bioavailable Vitamin D.
We all have a protein called Vitamin D Binding Protein that latches on to Vitamin D in our blood, keeping it unavailable for our cells. Some of us have a D-binding protein with a higher affinity for Vitamin D – and that is genetically determined.
In other words, two people with different measured levels of Vitamin D may have the same effective levels of Vitamin D based on genetic variation in D-binding protein. That means that the genetic risk score might not be capturing exactly what we think it is – limiting the validity of this analysis. Of course, all those observational studies linking low vitamin D levels to bad outcomes suffer from the same measurement problem.
Personally, I’m not a huge fan of vitamin supplementation in general – I recommend that my patients try to get their vitamins through the food they eat, and, in the case of vitamin D, through the sunlight they get while exercising a bit outside. Fortunately, summer is coming – go to it.
A version of this commentary first appeared on medscape.com.