Vitamin C, Zinc, or Both For COVID-19: A Randomized Trial
/A well-conducted study doesn’t support supplementation.
Wouldn’t it be nice if there was a treatment for COVID-19 that was safe, effective, cheap, and out of the control of faceless pharma executives beholden more to shareholders than to patients? The dream of such a magic bullet has led to a number of similar claims that a given drug, or supplement in some cases, has dramatic effects against COVID-19. We saw it first with hydroxychloroquine, but similar hype surrounded Vitamin D, ivermectin, melatonin, Vitamin C, and of course Zinc.
What made the claims so compelling were two things: one, a dose of biologic plausibility – biologists could argue that there was some underlying reason why a given vitamin would help – usually citing beneficial effects on immune function or a reduction in inflammatory cytokines. But more than that, these drugs had something of an underdog story. These unassuming agents, with us for decades – or longer – could become our most powerful ally against this scourge of a virus. Preliminary data was often breathlessly hyped – but, as I pointed out in regards to Vitamin D – we’d been burned before. Many of us wanted to see the randomized trials before we committed to any of these potential cures.
This week, we got one such trial, appearing in JAMA Network Open looking at the ability of Zinc and Vitamin C, alone or in combination, to shorten symptoms of COVID-19 in outpatients.
This was a 2x2 factorial design as you can see here. Patients were randomized to usual care or one of the three treatment arms in a roughly equal fashion.
I love a good factorial design. So many boxes.
These were outpatients, so we weren’t going to see a ton of hard outcomes. Rather the researchers used a rank-based symptom scoring method. Each day, participants were asked about four symptoms, which they rated on a scale from 0-3, giving a symptom score range of 0-12. The primary outcome was the time to halving of the symptom score – in other words if you start at a 4, the time it takes to get to 2. Or if you start at 10, the time it takes to get to 5. This is a bit of a weird outcome, since it assumes some mathematical equivalence where I don’t think any exists, but I suppose it’s as good as we can get.
Here are the symptoms over time for the entire study cohort – you can see a general waning of moderate symptoms (yellow) in favor of mild symptoms in green.
Overall, most people get better over time. That’s good.
But when you stratify by treatment, the time to 50% symptom reduction was basically the same across the board – about five and a half to six and a half days depending.
Symptoms not shortened by Vitamin C, zinc, or both.
Secondary outcomes
No individual symptom resolved quicker with Zinc, Vitamin C, or the combo. Basically the population looked like we’ve come to expect, a few days of fever, with lingering cough and fatigue.
Side effects
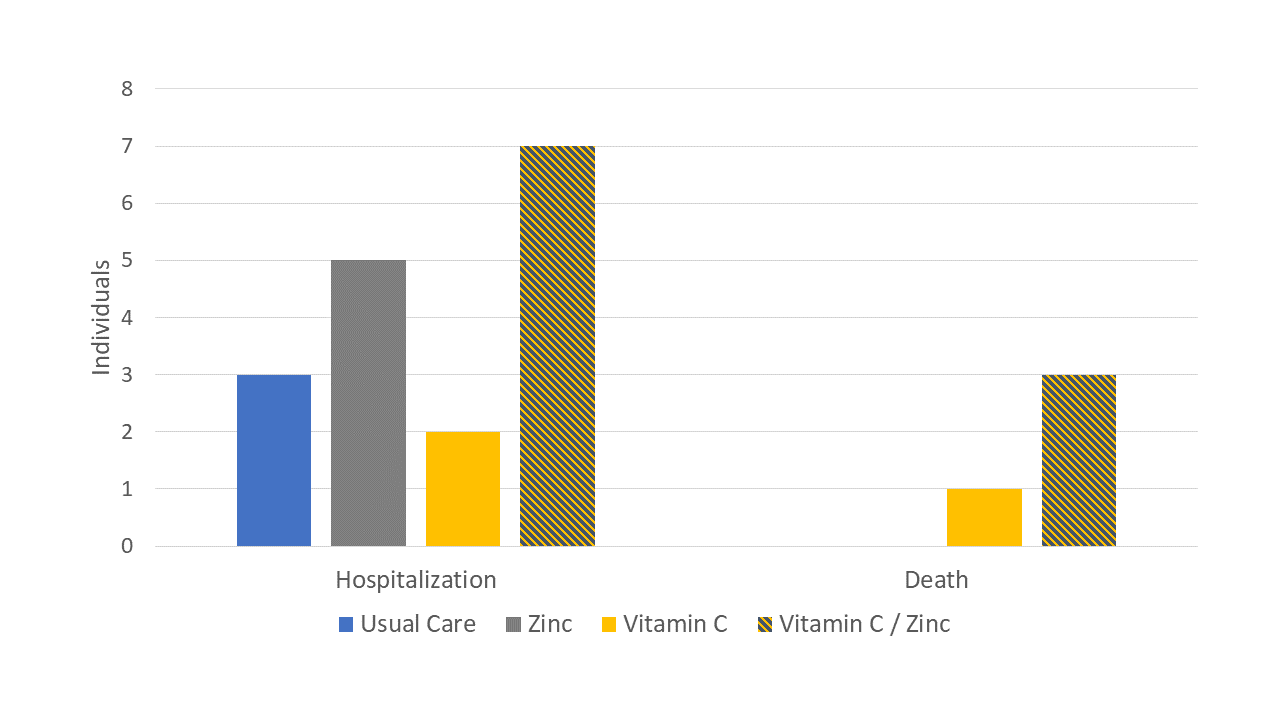
Hospitalization rate didn’t significantly differ, though it was slightly higher in the supplement groups. And there were thankfully only 3 deaths – 1 in the Vitamin C group and 2 in the combo group.
In terms of side-effects, nothing crazy but obviously the authors saw more in the treatment than the usual care groups. Mostly GI stuff.
Now, Zinc apologists will no doubt note the lack of a zinc ionophore (like chloroquine or pyrithione) as a reason this didn’t work and, again – I remind everyone that biologic plausibility is not the end of medical research but the beginning – it’s the minimum bar to pass to ethically conduct a definitive trial, not an end in itself. I’ll be happy to do a readout on any impending hydroxychloroquine zinc combo randomized trials that emerge.
More broadly, I think we need to just accept the fact that it’s pretty unlikely that a cure for COVID is sitting in our closets. Lots of chemicals have activity against pathogens in test tubes, just like lots of stuff works in vitro against cancer, but this trial reminds us that, more often than not, biologically promising agents don’t survive the rigors of real-world testing. Keep hope, but bring data.
A version of this commentary first appeared on medscape.com.