Emergency Room Visits: A New Way to Predict Thunderstorms?
/It’s no “trick knee” but ED visits for respiratory complaints spike before thunderstorms. What’s going on?
I had a friend once who claimed it was his special ability to be able to tell exactly when it would start raining. Like he’d look up at the sky and say “in 90 minutes, it will be raining”. This is not the most useful of talents in the age of meteorology but nevertheless I thought of him as I read this study, appearing in JAMA Internal Medicine, which found that ED visits for respiratory complaints spiked before a thunderstorm.
If you can’t describe your study with two icons it’s too complicated.
This was a large study. Researchers led by Anupam Jena of Harvard used the Medicare fee-for-service database to capture beneficiaries’ ER visits for a respiratory ailment from 1999 to 2012. They then combined this data with US National Oceanic and Atmospheric Administration weather data covering all 3,127 counties in the continental US.
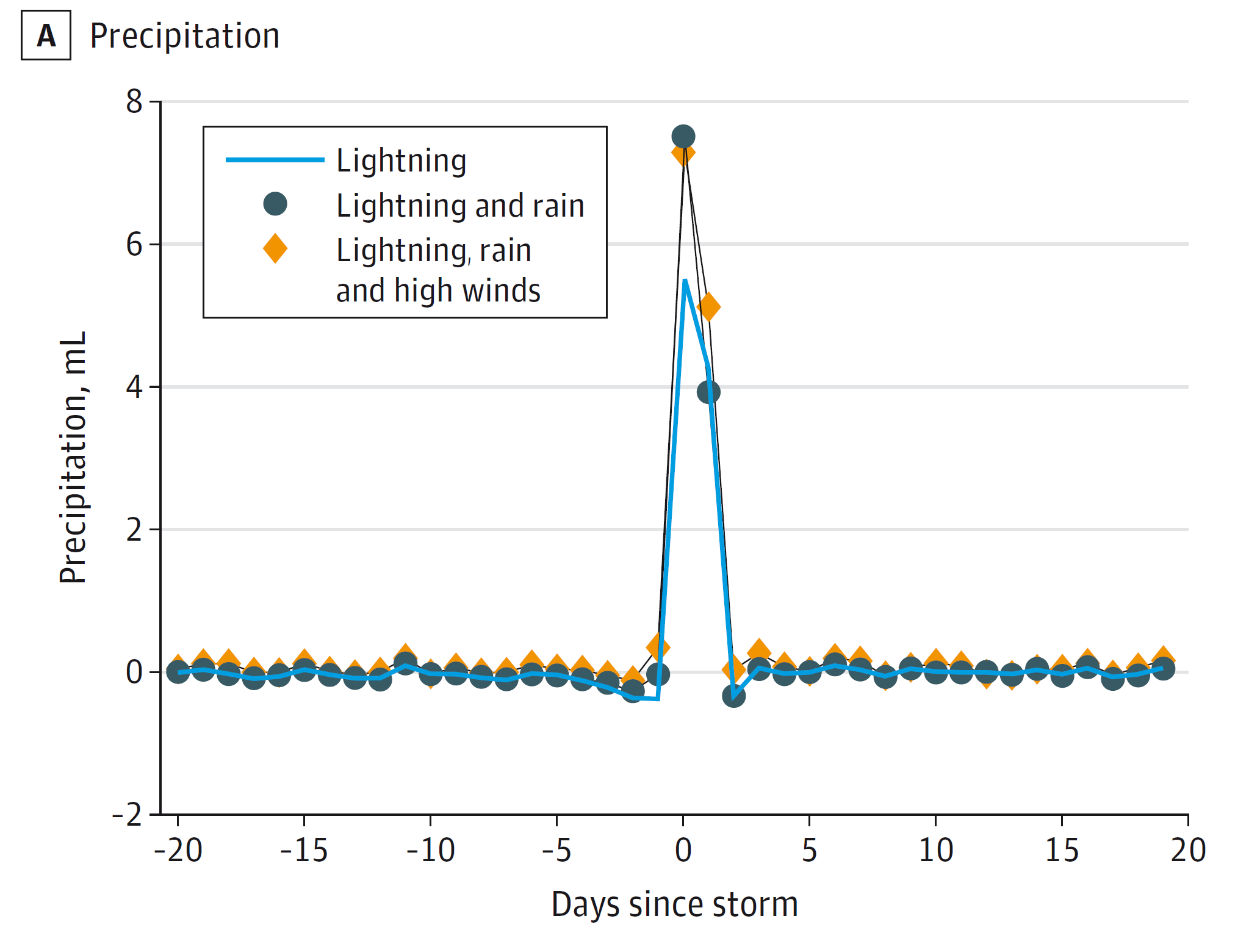
Precipitation seems to spike right on the day when a thunderstorm hits. Hmm…
They used that weather data to find days when counties had thunderstorms, defined in this case by high winds, lightning, and precipitation. With that storm as “time 0” they could look back and forward in time to see how ED visits stacked up. You can see that, as expected, precipitation spikes on a day that there is a thunderstorm. That’s proof of concept.
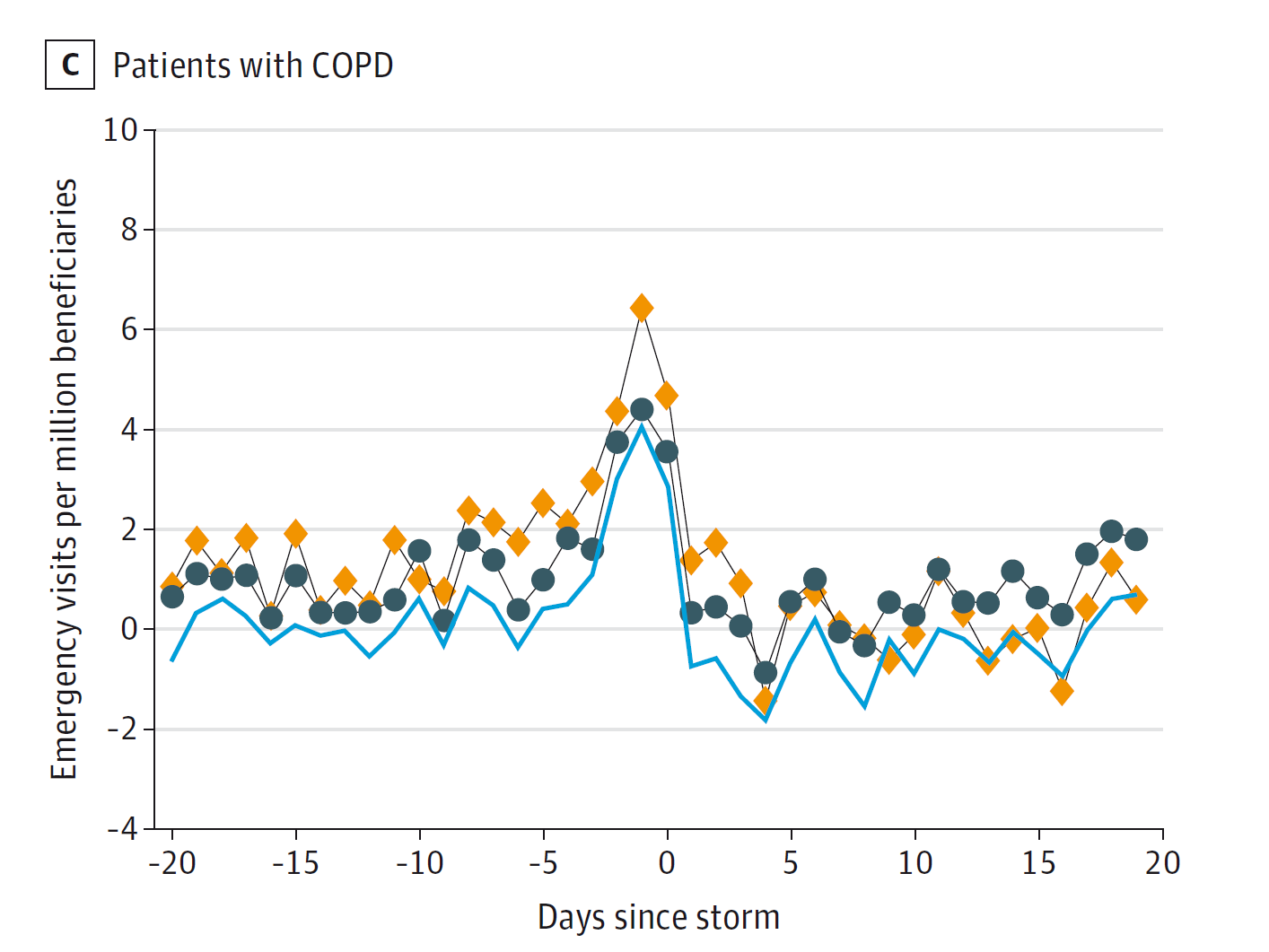
Now look at ER visits for respiratory complaints.
The relationship is actually pretty striking. You can see here a bump in ED visits for respiratory complaints occurring about a day before the storm. The spike is even more evident among those with preexisting COPD.
But ER visits for respiratory complaints spikes a day BEFORE the storm.
This is actually a bit surprising. Prior research has found an increase in admissions after storms – attributed to soaked pollen particles rupturing and spreading throughout the air after the downpour. Here we see the opposite. What’s going on? Are lungs like my friend, with the uncanny ability to detect rain in the near future?
Even more so if the patient has preexisting lung disease
Looking at other environmental factors, you can see that two things anticipate a thunderstorm – an increase in air temperature and an increase in particulate matter in the air. Maybe it’s not the storm at all then, it’s these presages of the storm.
Hotter temperatures have been shown to be associated with COPD admissions, as have higher amounts of particulate matter – so either or both of these could be contributing. I’d have liked to see some adjustment for these factors to see what is really driving these results, but we don’t get that in this particular study.
This is probably the culprit. Expect more as global temps rise.
Maybe people are trying to get themselves taken care of before the big storm hits? If so, we’d expect to see a spike in ED visits for other causes, but the negative controls in this study – sepsis and pulmonary embolism – had no association with weather events.
Why does this all matter? No, we should not use ED census as a way to predict the weather – meteorologists are still slightly better at that than we would be. Rather, this study reminds us that health, weather, and climate are connected. Wind, heat, and rain can have downstream effects on health conditions. As the globe warms, it’s fairly clear that we can expect more thunderstorms. We can also, possibly, expect more COPD exacerbations.
This commentary first appeared on medscape.com.