Prudes, Rejoice! A Study Links Number of Prior Sexual Partners to Cancer
/The BMJ Sexual and Reproductive Health article has us all rapidly tallying, but is it hot or not?
This week – the sexual history takes on new importance with a study in BMJ Sexual and Reproductive Health that suggests that the number of prior sexual partners you have is associated with your risk of cancer.
Full disclosure – I’m not a great sexual history taker. I basically ask if my patient is sexually active or not, and then I ask with men, women, or both. And then I’m done. As a nephrologist, I spend more time probing about how many prior NSAIDs they have taken than how many prior partners they’ve had.
But according to the BMJ study, number of prior partners may be a new risk factor of note. Well at least if the answer you get is “more than 10”.
While you’re all busy tallying, let’s dig into the study.
This is an analysis of the English Longitudinal Study of Aging or “ELSA” study, and I just can’t let it go.
Sorry.
Ok 2,537 men and 3,185 women provided information regarding their prior sexual partners and a complete description of their health status.
Big caveat here – only 67% of individuals in the ELSA study responded to the sexual history survey, and only 80% of those had complete details in terms of other health outcomes – so we’re in the land of biased samples.
Nevertheless, some interesting trends emerged.
On average, men reported having more partners than women. In general, younger age, being unmarried and being in the highest or lowest quintile of wealth was associated with having a higher number of lifetime sexual partners.
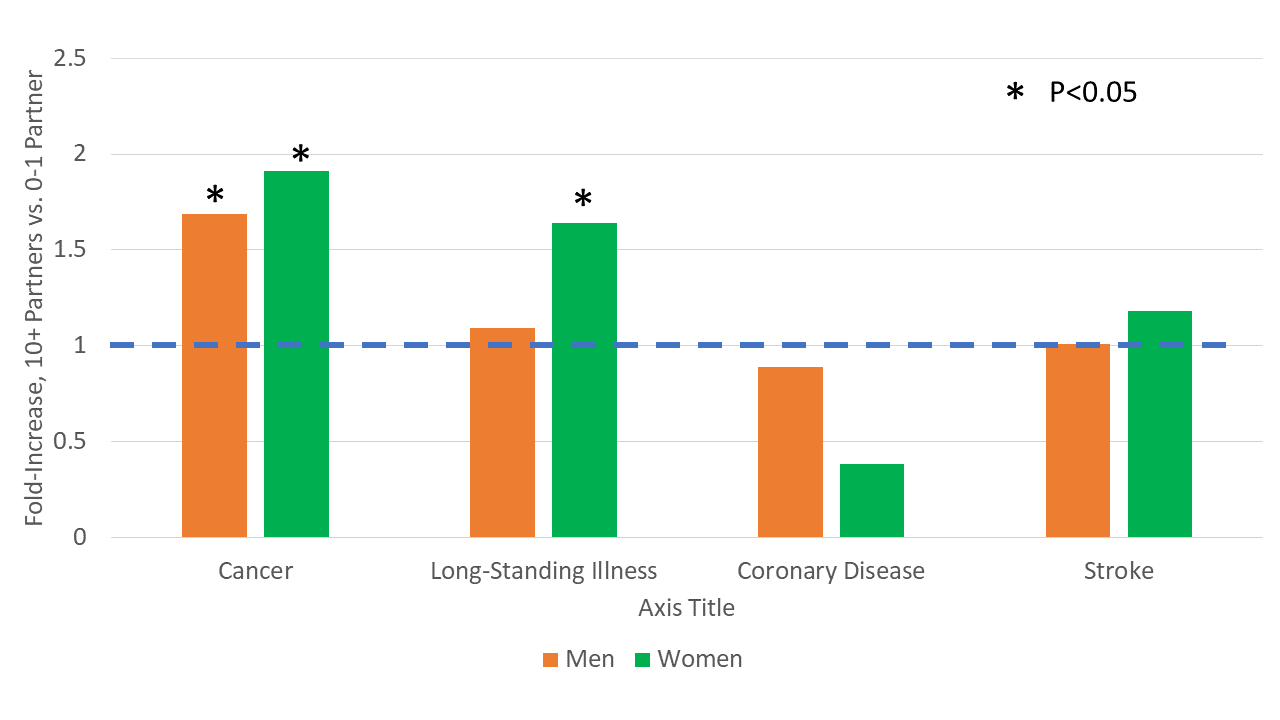
And, after accounting for age, partnership status, and a number of other factors, having a higher number of sexual partners was associated with a higher rate of cancer in men and women, and a higher rate of “long-standing illness” in women.
Why?
Well, the authors note that there’s a lot of data that suggests that having more partners increases the risk of sexually transmitted infections, and some sexually transmitted infections can cause cancer – we’re looking at you HPV. Seems plausible.
But this is a long way from confirmed – first of all, we don’t know what TYPE of cancer these people had.
But… the signal to noise would be higher if you restricted to cancers caused by STIs, right?
The authors write that there are too few cases to do a formal analysis by cancer type, but that rings a bit false to me, since, presumably, all the lung cancers and breast cancers and stuff are just noise in the system – restricting to cancers we know are associated with STIs should show a strong signal if there’s causality here.
No probably what we are seeing here isn’t the lifetime downstream sequela of STIs. We’re seeing our old friend confounding rearing his confusing head.
I’m going to give you the D. By which I mean Directed Acyclic Graph
Women and men with a history of more sexual partners are bound to be different in a host of ways from those with few or no sexual partners. And you can’t adjust for everything – education was a notable variable missing from the multivariable adjustment for example.
Despite that, you and I both know that this study will creep its way into some abstinence-only education class, or some other puritanical effort to stigmatize sex.
And that’s not good. A different paper from the same dataset examined the effects of sex on happiness in the same population, and you know what?
Those who had more of it were happier.
Happy Valentine’s day.
This commentary first appeared on medscape.com