When the First Antidepressant Fails... A Randomized Trial
/For the video version, click here.
Major depressive disorder affects 16 million Americans, and treatment is difficult. We often find ourselves in a position to re-evaluate a patient, treated with a first-line antidepressant, who has not achieved remission. Where to go from here?
Researchers in the Veterans Affairs system took on this question in an ambitious three-arm trial, appearing in the Journal of the American Medical Association.
Here’s the setup. They identified 1,522 patients with major depression who had not responded to at least one course of antidepressant. Most of these, as you would expect, had tried an SSRI. And the majority were currently receiving psychotherapy. Researchers randomized these individuals to three different treatment strategies.
One – switch the current drug to bupropion, a norepinephrine-dopamine reuptake inhibitor. Two – add bupropion to whatever they were already taking. And three – what might seem a bit unorthodox to those of us who don’t treat a lot of depression – add aripiprazole – a second-generation antipsychotic.
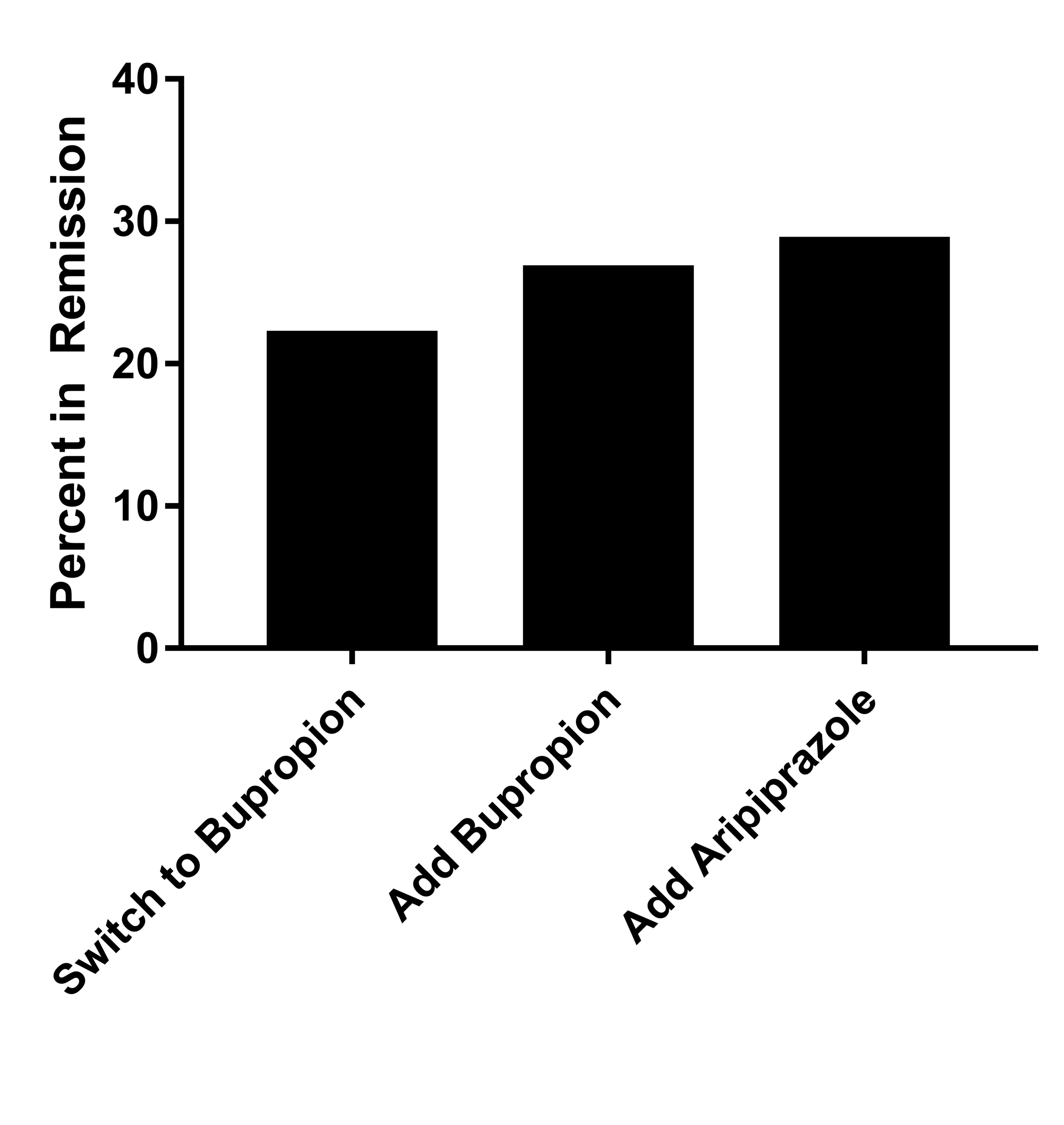
The primary outcome was remission of major depression. Consistent with many depression studies, the rate of remission was disappointingly low in all three groups.
Only 22% of those who switched to bupropion got into remission compared to 27% who had bupropion added. Roughly 29% of patients getting the antipsychotic achieved remission. The only statistically significant difference here was between the aripiprazole group and the switch group.
Moving on from full remission, the authors also examined which strategy would associate with a significant reduction in symptoms. The antipsychotic strategy performed better than both other strategies in this analysis.
But aripiprazole has a bit of a rougher safety profile than bupropion, so we might not be too eager to go shopping in the antipsychotic aisle for depressed patients.
Unsurprisingly, weight gain was substantially higher in the aripiprazole arm as was somnolence, akathisia, and extra-pyramidal symptoms. Those who got bupropion tended to get a bit more anxiety and jitteriness – again not surprising considering the stimulant effects of that drug.
We also need to remember the population here. These patients were recruited from VA hospitals, and, as a VA physician myself, I can tell you that depression in veterans feels a bit different than depression in the general population. The comorbidities of PTSD and other medical conditions may have given a boost to the benefit of aripiprazole that we might not see outside of this specialized scenario.
In my personal opinion – these results are not robust enough to recommend the routine use of adjunctive aripiprazole over other more benign medications. But obviously, this will differ from patient to patient. What is clear, though, is that there are real options for those who fail to achieve remission after first line therapy.