Black Kids More Likely to Die After Surgery White Kids
/What really matters, race or racism?
In my day job, I’m a clinical researcher and do a fair amount of statistical modeling. When I got started maybe 10 years ago, there were three variables that you had to put into any model you made. Age, sex, and race. You had to adjust for those three things. It was pretty standard. There’s an implicit assumption there – that those things – age, sex, and race, drive outcomes of interest and thus need to be taken into account. But early on I never gave it much thought. Why does race drive outcomes of interest? And of course, the more you ask yourself that question, the more you realize that the thing you should be adjusting for isn’t race at all. It’s racism.
This issue has been brought to light again in this study, appearing in the journal pediatrics.
Let me start at the end. This study shows that among healthy children undergoing an inpatient surgical operation, black kids have a 3.5-fold increased risk of perioperative mortality compared to white kids.
That’s enough to write some compelling headlines, but let’s dig in to the study a bit. Researchers used the massive American College of Surgeons National Surgical Quality Improvement Program (NSQIP) pediatric database to examine operative outcomes in over 170,000 operations in the US.
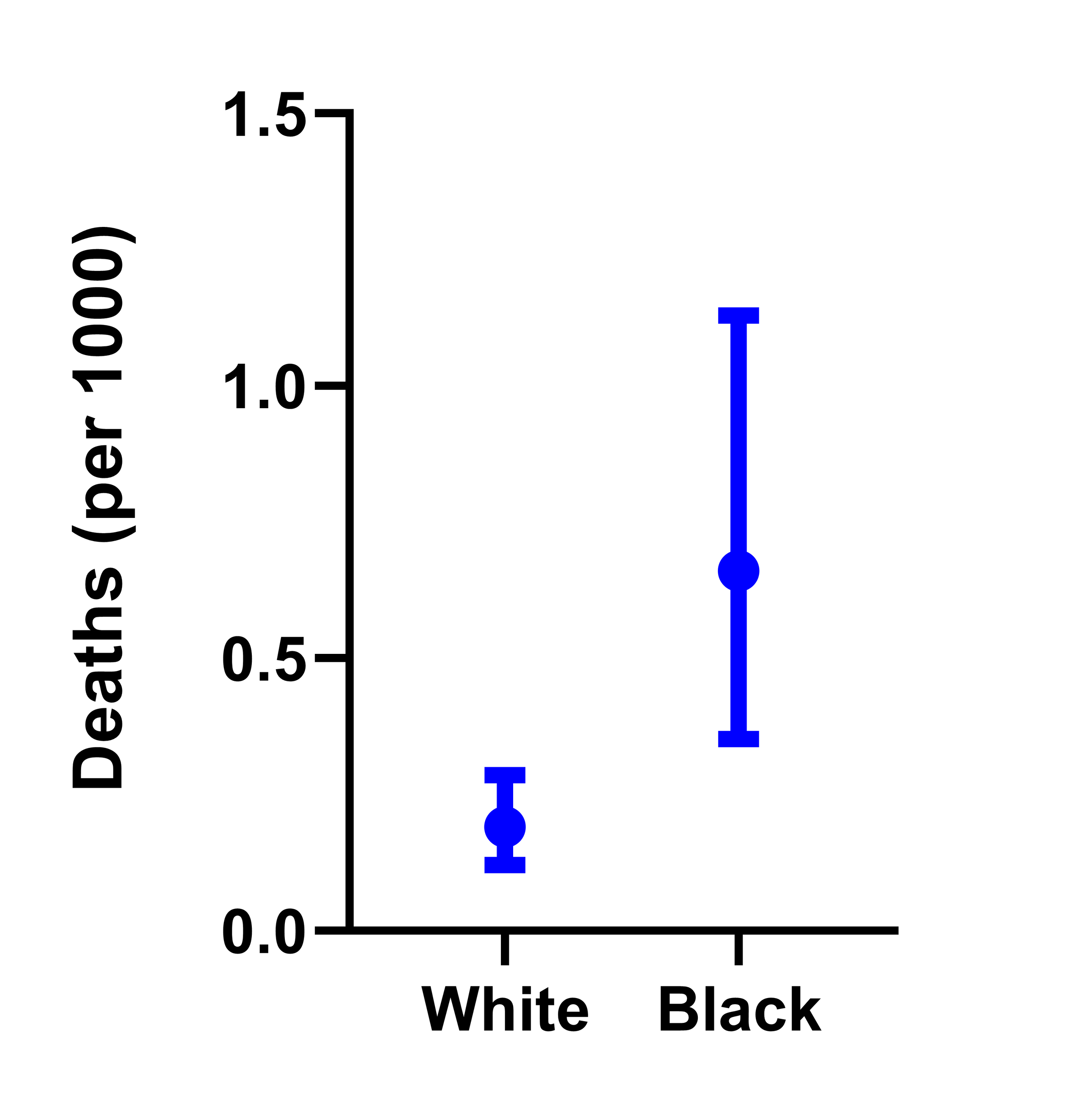
Post-operative mortality rate shows a small, but significantly higher risk among black kids.
Now, to be sure, post-operative deaths in healthy kids aren’t common. Out of 120,991 white kids who had an operation, there were 23 deaths – 0.02%.
Of 19,675 black kids in the study, there were 13 deaths 0.07%. But this difference was large enough to achieve statistical significance. It also withstood statistical adjustment for age, sex, the year of surgery, whether the surgery was elective or emergent, the operating time, and the RVUs associated with the procedure (which is sort of a marker of surgical complexity).
Researchers found a similar directionality of relationship between race and 30-day complications and serious adverse events, though of lesser magnitude. Black kids were around 20% more likely to have a complication and 7% more likely to have a serious adverse event.
ASA Categorization
Adjustment for various surgical factors doesn’t seem to modify the risk estimate too much.
These are not entirely new findings, but research in the past has attributed the disparity to a higher burden of comorbidity among black children. The researchers in this study got around that problem, by only including kids who had American Society of Anesthesiologists Category of 1 or 2 – totally healthy, or with a mild condition (like asthma) that was well-controlled.
The ASA score could have been under-reported of course. But prior research has shown systematic OVER-reporting of ASA scores in black kids. In other words, that means the black children analyzed in this study would have been systematically healthier than the white kids, making the disparity in outcomes that much more stark.
So… why? I opened this commentary saying that we need to worry less about race and more about racism and I stand by that. But I’m not really talking about explicit racism here – caregivers deliberately taking worse care of black kids. Implicit bias is a real problem, as some papers looking at adult surgical care have suggested. But there are structural elements here too that we need to think about. One missing covariate is the type of hospital that did the surgery – access to high-quality medical centers and health care is a form of institutionalized racism that needs to be addressed by smart policy. Differential insurance plans or the delay of care for Medicaid patients, who are more likely to be black than the general population, are other systemic processes that impede good care.
Yes, some of this is poverty. The authors did not adjust for household income. But I want to be careful to not let race be subsumed by class. There is an understandable temptation to attribute observations of race-based disparities to class-based disparities since, frankly, the latter seems more fixable. And while race and income are correlated, they are not collinear, and multiple studies that have investigated the impact of race AND income in the healthcare setting still show that race is an independent risk factor for bad outcomes.
Our duty as healthcare providers is to provide the best possible care to every person sitting in front of us, or lying on our operating tables. But we need to realize that by the time the patient gets to us, some damage may have been done. The first step to improving disparities in outcomes, is acknowledging that racial disparities exist. I wonder if a study of healthy children like this might drive home that point more than the myriad of studies that have come before.
This commentary first appeared on medscape.com.