Doc Ratings Driven Strongly By Willingness to Prescribe Antibiotics
/A new study suggests that prescribing antibiotics for upper respiratory infection leads to a significantly greater chance of a “five-star” review.
This week – have you googled yourself lately?
If so, you may have noticed a few stars under your name. There are multiple websites that offer patients the opportunities to rate providers, and I think we all take these reviews pretty seriously.
In a competitive market, a five-star rating can make a big difference.
Wow, what a talented breast surgeon that must be.
Now a new study in JAMA Internal Medicine provides the secret to higher patient ratings.
That secret? Prescribe antibiotics.
Researchers from the Cleveland Clinic used data from an online telehealth service called Amwell that provides rapid access to physicians for urgent issues via a smartphone or tablet.
Importantly, after the interaction with the physician, the patient rates their experience from 1 to 5 stars.
Over a 6-month period, 85 physicians had 8437 encounters with patients for upper respiratory infections. Now as we all know but frequently forget in the heat of the moment, the vast majority of URIs are due to viral infections. Nevertheless, 66% of these visits resulted in an antibiotic prescription.
And patients liked that a lot.
91% of patients who got an antibiotic prescription rated their encounter at 5-stars compared to 73% of those who didn’t get a prescription. Those who got a non-antibiotic prescription were somewhere in the middle.
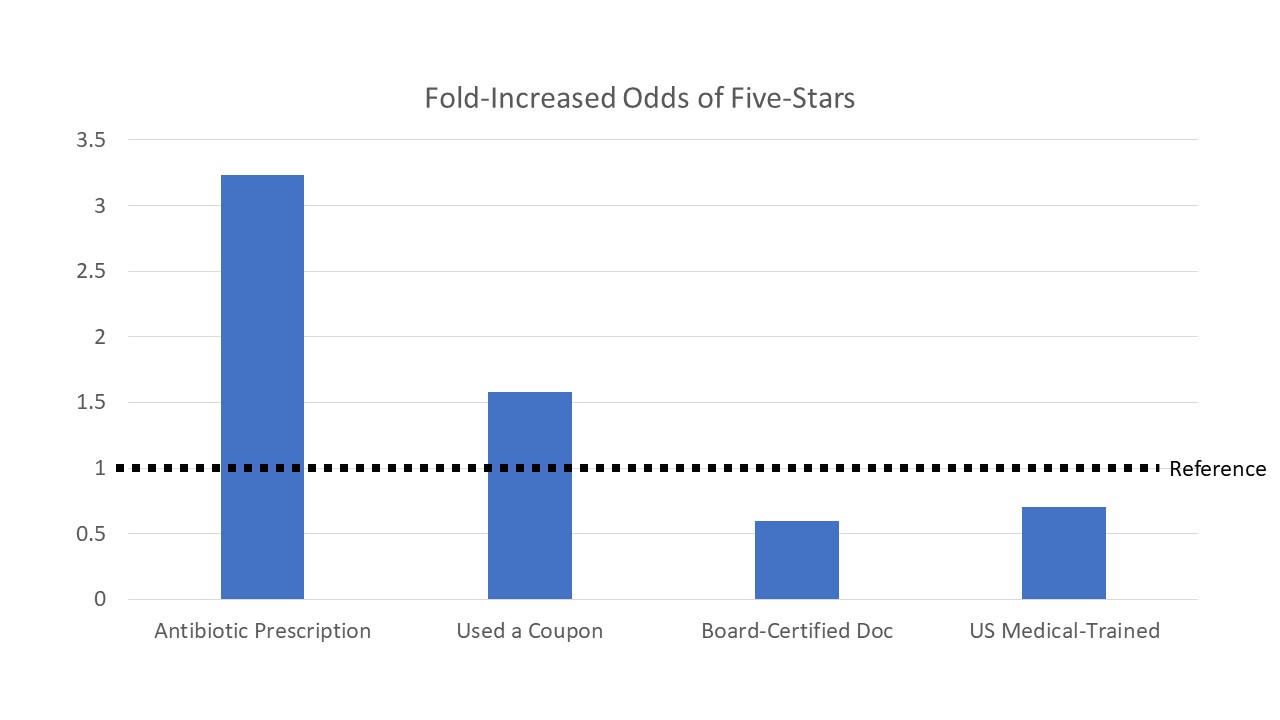
In fact, when the researchers looked at predictors of a 5-star rating, nothing came close to that antibiotic prescription.
Even having a coupon for care couldn’t match the positive power of the prescription pad.
What I like about this study is that it lays bare a rather uncomfortable truth. We want our patients to like us. And sometimes that desire is in conflict with our other obligation to do no harm.
Speaking personally, I’ve justified this line of action to myself by thinking – yeah, I know this antibiotic isn’t really going to help, but the placebo effect will help and the risk of a bad reaction to the drug is low and hey, maybe it has some anti-inflammatory properties and one prescription really doesn’t matter.
And that’s all true – but it’s like that new dance “the floss”. When one person does it, its ok. When we all do it, there’s a problem.
Some caveats here – this is one company marketing directly to consumers so the behavior of these docs may reflect a particular focus on patient satisfaction. But I don’t think the results are terribly surprising.
I will say I’m encouraged by the beneficial effect of non-antibiotic prescriptions here actually. If you don’t want your ratings to suffer too much, but don’t want to contribute to an epidemic of antibiotic resistance, providing a non-antibiotic prescription may thread the needle quite nicely.
Of course, the elephant in the room here are the rating systems themselves. Do they help patients find the best doctors for what they need or do they help patients find the best doctors for what they want. The answer is in the stars.
This column originally appeared on Medscape.com.