Coronavirus: Endgame
/It’s time to start defining our criteria for victory over COVID-19.
After what we’ve all been through, it sounds almost crazy to talk about – but we really should start thinking about what we would call “victory” in the fight against coronavirus.
Lately, there have been a slew of think-pieces about when life will get back to normal, but that’s not really what I want to talk about. I’m thinking farther into the future, 5-years, 10-years. What are the potential scenarios? And what can we honestly say means we won?
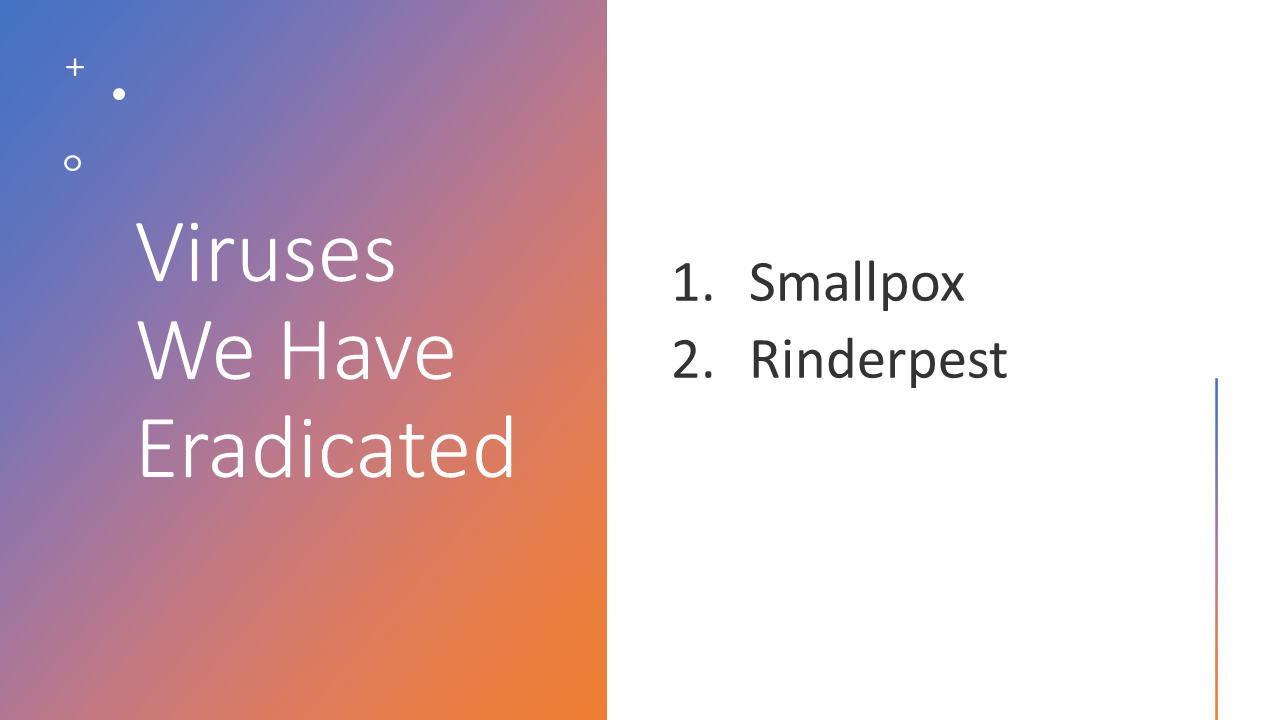
I’ll start with the clearest victory – total SARS-CoV-2 eradication. The hashtag #zerocovid is certainly catchy, but even proponents would be quick to tell you that #zerocovid means elimination, not eradication. What’s the difference? Eradication means that the virus has ceased to exist in the world, except perhaps in certain labs. Here is a comprehensive list of viruses that the human race has eradicated.
Rinderpest only infects cattle, by the way. Or it did. We eradicated it.
The reason we could eradicate smallpox was two-fold. One, we had an effective vaccine. Two, there were no animal reservoirs of the disease (it probably jumped to humans from rodents 50,000 years ago, but in modern times we were the only vector). That meant a global vaccination project could achieve eradication. And it did.
We have an effective vaccine (multiple, in fact) against SARS-CoV-2, but we also have the pesky problem that the virus can circulate in other mammals. It’s hard to catch and vaccinate all the bats. So another species jump is always possible.
Can we move from eradication, then, to elimination? Here the idea is that there is no acceptable limit of COVID cases. We get the rates as low as possible and then, when an outbreak inevitably occurs, we stop it from spreading. Think firemen putting out a housefire before it spreads to the whole neighborhood.
Possible? Maybe. But the problem – the secret weapon of COVID-19 – is asymptomatic spread. By the time we see those first cases, the horse might be out of the barn. Or, to avoid mixing metaphors – the invisible fire may have already spread?
This is the fundamental public health difference between SARS-CoV-2 and the more lethal SARS-CoV which was responsible for the SARS outbreak in 2002. Also a virus with an animal reservoir, we haven’t had a single case worldwide since 2005. If not eradicated, SARS was eliminated. This was possible, in no small part, because people were almost universally symptomatic while they were infectious. Remember the temperature screenings at airports? They work – if people who are infectious actually have fevers.
So while elimination is aspirational, I don’t think we should set the bar for victory quite that high.
The next level I’ve seen tossed around isn’t ambitious enough though.
This is the idea that if we can get COVID cases to look more like the flu, we win.
Let’s put some numbers to it. Flu deaths are variable, but tend to kill about 25,000 individuals in the US each year. That works out to 68 a day. Currently, even with death rates falling, we’re seeing around 2500 COVID deaths a day.
Some experts have said that if we can get COVID-19 deaths down to below 100 a day in the US, we’ve done as good as can be expected. We’ve transformed a raging scourge to another flu.
But here’s the thing – I don’t want another flu. If COVID never existed, but flu suddenly got twice as deadly, wouldn’t we all be freaking out? This bar is too low for me.
And I think we can do much better. In fact, for multiple reasons, I think we can get “endemic COVID” to rates much lower than endemic flu.
First, we have the vaccines. Flu vaccines vary year to year but tend to have about 50% efficacy – good, not great. The coronavirus vaccines have dramatically higher efficacy rates – up to 95% for the mRNA vaccines, and are even more protective when it comes to severe disease and death.
Second, flu is a fickle virus. Though the mutation rate of Influenza A isn’t as dramatic as some of the great mutators like HIV and HCV, it is dramatically higher than SARS-CoV-2, thanks in part to a proofreading enzyme that the coronavirus carries in its genetic makeup.
Mutation rates (nucleotides per cell infection) for selected viruses
Why then, are we seeing all these variants? Simple, every cell infected is a chance for a new mutation to occur – more people infected, more cells infected, more mutations, even with a virus that, on its own, is pretty stable. The implication is positive – if we can squelch the infection rate, the virus won’t be able to evade our defenses as quickly – giving us a chance to keep it good and squelched, even more so than we do with flu.
The third edge we have against COVID-19 is its weird spreading pattern, though it’s a double-edged sword. By now, we’ve all basically memorized that the R0 of SARS-CoV-2 is 2.5 or so, much higher than flu which is usually in the low 1s. But the idea that each infected person infects 2.5 additional people is just an average. COVID spread is considerably clumpier than that, with superspreading events driving a lot of transmission. This can be quantified by the k-number – the dispersion parameter. Flu A has a K of around 1 – meaning spread is pretty uniform. SARS-CoV-2 has a K of around 0.1, meaning that a small number of people are responsible for a large number of cases.
This could be good for us. It means that, if we can get rates way down, we are more likely to see isolated outbreaks that we can quickly pounce on compared to the slow-burn that we see in a typical influenza season. Of course, one big super-spreading event in an indoor concert or something would set us way back.
Flu vs. Sars-CoV-2
My belief, if we do this right, is that 5-years from now, we’ll still have coronavirus, but cases may be extremely rare – worthy of particular attention – local, regional, and national reporting – that sort of thing. We may not give it the smallpox treatment or the polio treatment, but it certainly doesn’t have to be another flu.
A version of this commentary first appeared on medscape.com