Antidepressants in Mothers, Autism in Children: The Data
/For the video version, click here.
Towards the end of 2015, an article appeared in JAMA Pediatrics linking maternal use of antidepressants with autism spectrum disorder in offspring. The media reaction was predictable:
A few voices of caution emerged though, most noting that the 87% increased risk of autism seen in that study was a “relative” risk. The absolute risk of autism was 0.7% among moms not taking SSRIs and 1.2% in those who were, so really the risk was quite small no matter what.
But even those sober arguments gave weight to the results – there is risk there, however small it may be. And when it comes to their children, parents don’t really embrace the concept of tolerable risk. We need to be cognizant of the big picture here. It is vital we determine the causes of autism, and equally vital that we be very measured in our assessment of any study. After all, we’ve been burned in the past.
If you’re a diehard fan of my blog, you’re probably my mom and you may remember a younger version of me reporting on this earlier study:
I should be careful what I wish for. This week, we have a trio of new studies, all asking the same question, using different data sources. And all doing a better job adjusting for those pesky confounders than prior studies. But the verdict is mixed.
First up, this study examining the association between antidepressant use and autism spectrum disorder in a large Ontario registry:
There are no surprises in the unadjusted data. The risk of autism spectrum disorder among the 2,837 children exposed to SSRIs during pregnancy? 2%. The risk in the roughly 33,000 unexposed kids? 1.1%. Similar numbers to the 2015 data, again with that frightening “doubling” of risk.
Things get more complicated after adjusting for important factors like maternal age, prior psychiatric history, and a slew of administrative codes. Using traditional multivariable adjustment, SSRI use during pregnancy was still associated with a 59% increased risk. Case closed?
Nope. Because using inverse-probability weighting, that association lost statistical significance. Inverse probability weighting is a statistical technique that gives more importance – weight – to points in the data that are more surprising. So a mom taking anti-depressants despite having none of the risk factors you’d expect gets counted more than the mom with a long depression history or other factors that predispose to antidepressant use.
Why do this? Well, the idea is that by weighting the “surprising” patients more, you get a better sense of causality – after all, these people don’t have any of the classic factors predisposing to antidepressant use, so if their kid develops autism, you might feel it’s more appropriate to blame the antidepressant.
Using this form of weighting, the Ontario study still shows an increased risk of 61%, but the confidence interval ranges spans 0% added risk. Technically, this makes the association between SSRI use and autism spectrum disorder not significant. But boy is it far from reassuring.
See, the problem is that the more factors you adjust for, the wider the confidence interval gets. So you can make a significant finding non-significant just by adjusting for a million things – it shouldn’t necessarily convince you that there isn’t a causal agent at work.
The next study used Swedish administrative data encompassing more than 1.6 million births and a similar approach:
What's going on in Sweden?!
The raw data was a bit surprising here. Among those exposed to antidepressants during pregnancy, the risk of autism spectrum disorder was 5.3% compared to 2.1% in those not so exposed.
There’s that doubling again, though I can’t help but notice the significantly higher baseline rates in Sweden compared to Canada. I will say the Canadian study had more strict diagnostic standards.
After adjustment for things like maternal age, suicide attempts, and level of education, the risk of autism spectrum disorder was about 66% higher in the exposed group.
But these authors did something clever. They knew they couldn’t adjust for all the important factors, so they compared disjoint siblings. In other words, they found families where one kid was exposed to antidepressants in utero, and a sibling wasn’t. If antidepressants were causative, you’d see a higher rate of autism in the exposed sibling. They saw no such relationship. This suggests that genetic and shared environmental factors might drive both an increase in antidepressant use and autism, and the drugs themselves are off the hook.
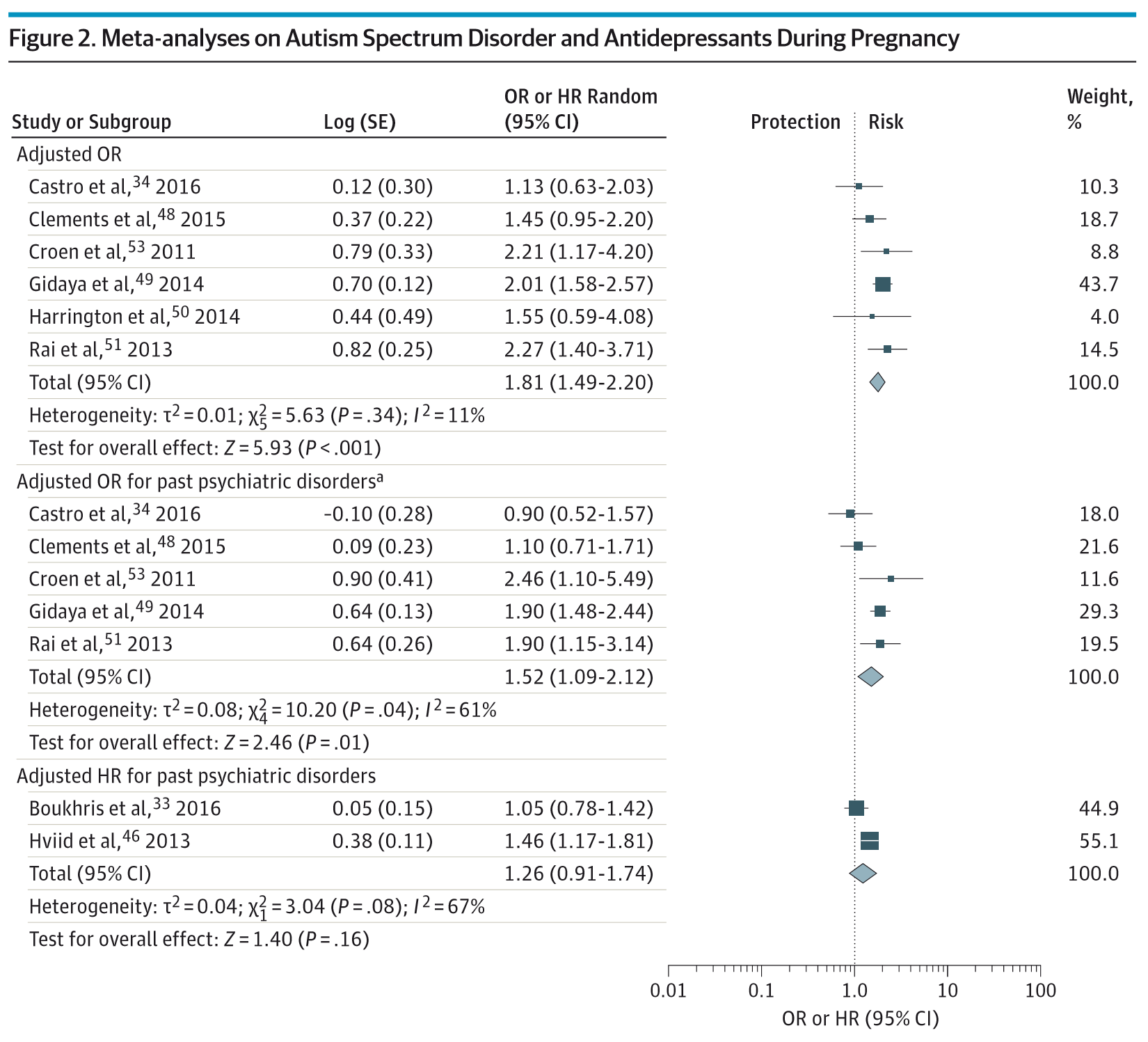
Finally, this meta-analysis, synthesizing the extant literature – though not, importantly, including the two studies I just discussed.
There are a lot of analyses here, but the authors basically arrange their results by how many confounders were accounted for in the various studies.
The bottom line? The better the studies adjusted for confounders, the smaller the association between antidepressant use in moms and autism spectrum disorder in children.
So let’s put this all together. It’s clear, really beyond a shadow of a doubt, that women who take antidepressants during pregnancy are more likely to have children diagnosed with autism spectrum disorder. What’s not clear at all, is whether the antidepressants themselves cause the syndrome. In fact, the sibling analysis argues very strongly against that.
So when a patient brings up this data, the important thing is to keep perspective. The risk of autism spectrum disorder in a child is quite low regardless of whether you use anti-depressants or not.
And stopping an anti-depressant can have serious consequences with regards to peri- and post-partum depression risk. So that decision needs to be made with sober heads, and all the information we can muster.