Rosacea linked to Parkinson disease: Is this remotely plausible?
The title of the manuscript is: 
Titles like that remind me of the time I was in South Africa and ran into an evangelical Christian basketball team. I know what both of those things are, but I’d never thought of putting them together. Nevertheless that’s the study that appears in JAMA Neurology. So are we playing epidemiology roulette, or is this a real finding? Should your patients with rosacea be concerned?
For the video version of this post, click here.
First things first, this is a study out of Denmark, a country with a nationalized and central health care system. Researchers examined… well… everyone in the country over age 18 from 1997 to 2011, so over 5.5 million people. They identified around 68,000 individuals with rosacea based upon either administrative codes or having received two prescriptions of topical metronidazole. They identified individuals with Parkinson disease based, again, on administrative codes. A sensitivity analysis looked at all those people who got medications associated with Parkinson disease, like levodopa.
Overall, those with rosacea were twice as likely to subsequently receive a diagnosis of Parkinson disease. After adjustment for a fair amount of covariates, the risk was lessened but still significant. Of course, that’s a relative risk. In absolute terms we’re talking about rosacea increasing the risk of Parkinson Disease from 3.5 cases per 10,000 person-years to 7.5 cases per 10,000 person years.
So… why? Well, the authors note that rosacea is associated with upregulation of a group of proteins called matrix metalloproteinases (MMPs) which have a role in tissue breakdown and repair. There is also a mouse model of Parkinson disease that shows upregulation of MMPs. A prior observational study of 70 patients with Parkinson disease showed a higher than expected rate of rosacea. But basically, that’s it. This is the first large, epidemiologic study to even examine the association between these two conditions.
Now I could mention that administrative codes are poor at capturing conditions like this, that people with rosacea may have more contact with the healthcare system and thus be more likely to receive a diagnosis of Parkinson disease, and that the study lacked a negative control condition – say Alzheimer’s dementia – to lend support to the biologic plausibility argument. But I don’t want to be cynical. This paper clearly represents the first foray into an area that probably warrants a deeper look.
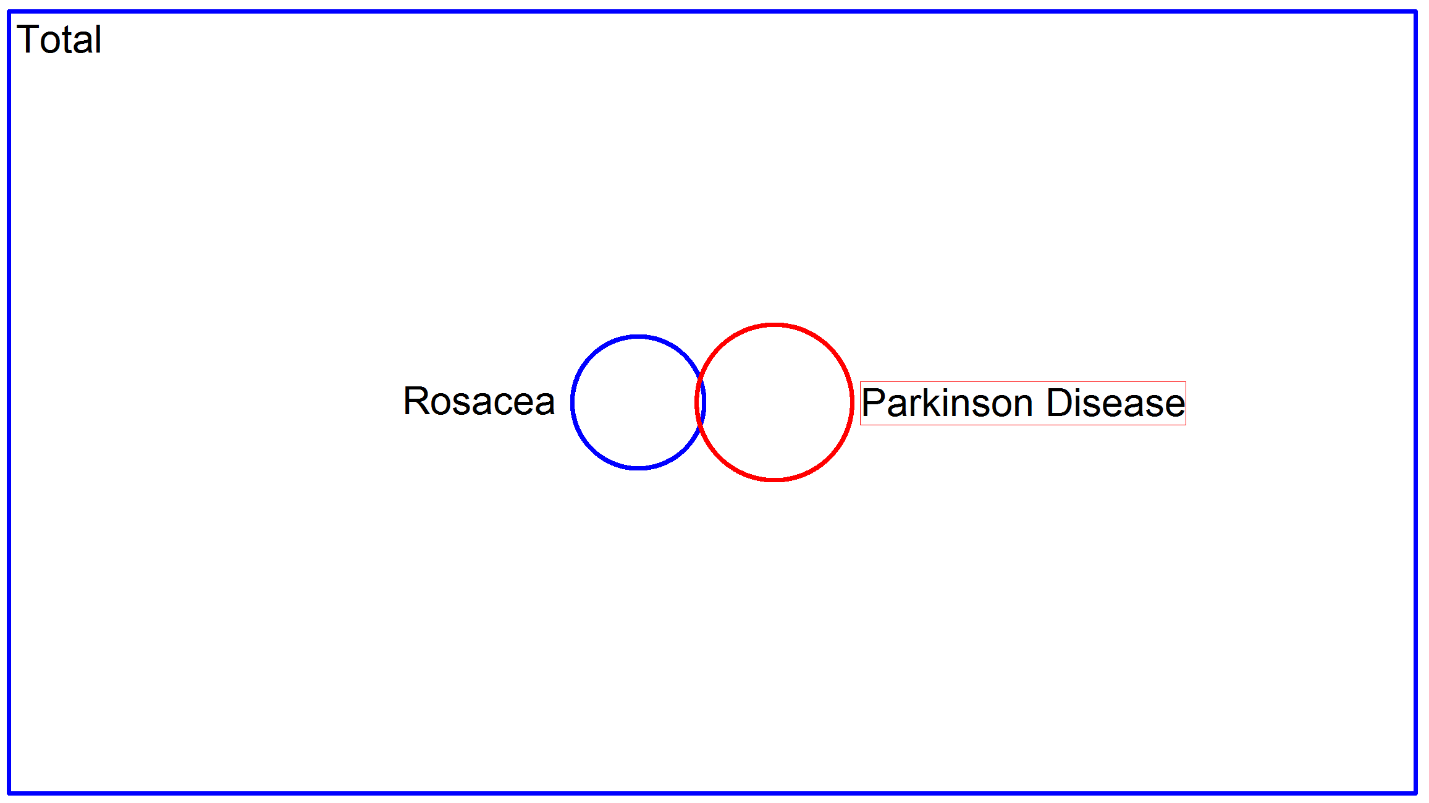
The important thing to remember though, is that even if this is a real finding, the impact for your patients with rosacea is quite minimal. I took the liberty of making a proportional Venn diagram here which I think is illustrative:
The big blue rectangle represents the total population of Denmark, and the circles represent the two disease conditions. There is some overlap between rosacea and Parkinson disease, but I think it should be very clear that most patients with rosacea needn’t worry. It is for this reason that I take issue with this statement: