For-Profit Dialysis Units Much Less Likely to Get Patients Transplanted
/In a really concerning analysis, researchers found patients are about half as likely to get a kidney transplant if they are receiving dialysis in a for-profit, compared to a not-for-profit unit. Hmm….
This week, try the following experiment. Find a nephrologist like me and ask them “what type of renal replacement therapy would you want if you needed it?”. If any of them say anything except “transplant” I’ll eat a cellulose semipermeable membrane.
That’s because transplant is demonstrably the best therapy for someone with end stage kidney disease. It’s cheaper than dialysis, less burdensome than dialysis, and is associated with longer survival than dialysis.
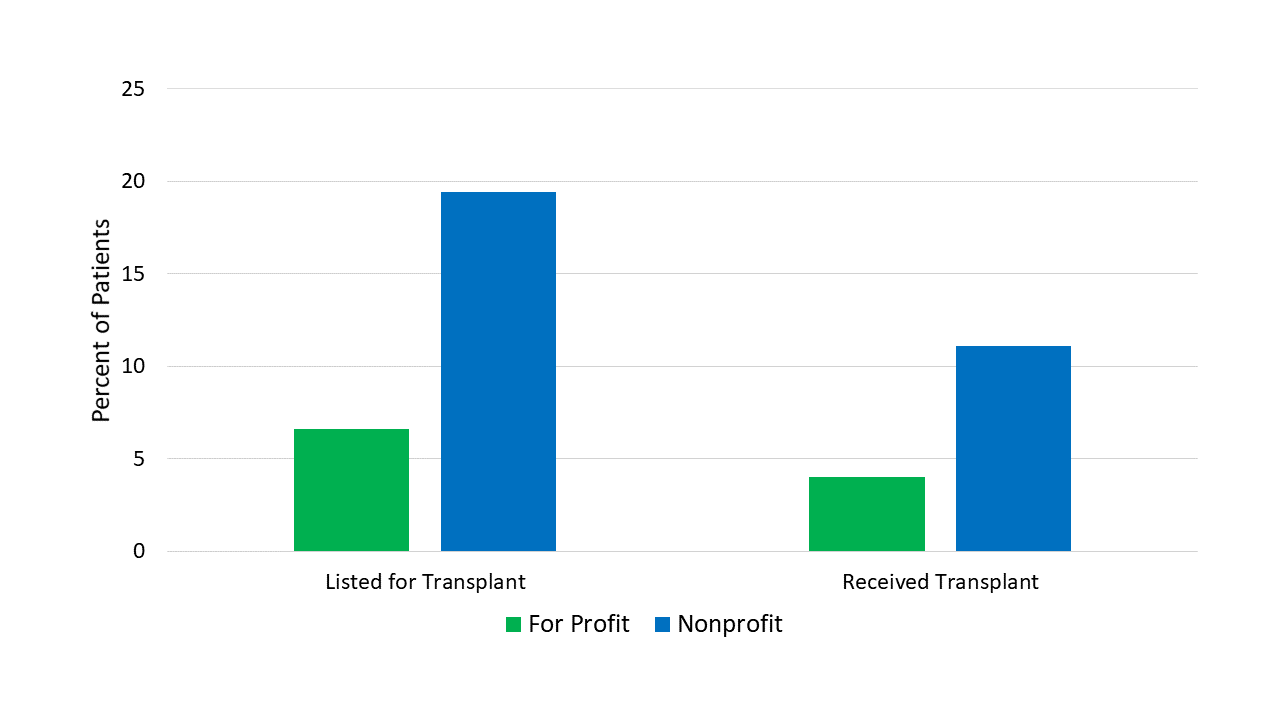
That’s why it’s so depressing to see this study, appearing in the Journal of the American Medical Association, which finds that in the US, just 8.2% of 1.5 million dialysis patients were placed on the transplant waiting list.
Only 4.9% ever got a transplant. This is bad. But it gets worse.
The for-profit chains are in green. Get it?! Design!
The study, which spanned from the year 2000 to 2016, took data from the USRDS – a national registry of every dialysis patient and linked it to two dialysis facility data sets. In that way the authors could look at these 1.5 million people and know what type of dialysis center they were in. As you can see here, the vast majority were treated at 1 of the 2 large national for-profit chains, with a smattering of patients treated at other for profit units and a minority – just about 13% treated at non-profits.
For-profit CEO: *sweats
Marketing guy: Case-mix!
Does it matter where you get treated? Apparently so.
Individuals receiving dialysis at for-profit chains were about 60% less likely to be put on the transplant wait-list than those at not-for-profits. They were half as likely to actually get a transplant.
Pitchfork time? I asked senior author Dr. Rachel Patzer of Emory whether the data showed that for-profit centers were potentially dragging their feet on transplant referrals in an effort to keep dialysis chairs filled:
“We certainly need more data to support these hypotheses, but it doesn’t look great for the for-profit facilities”.
-Rachel Patzer, PhD - Emory Univeristy
No it doesn’t. But Dr. Patzer was quick to point out that her study only captures a couple of steps in the transplant process – it takes a lot of things to get a kidney transplant.
Just a few of the steps it takes to actually get a kidney transplant.
Educating the patient about transplant, agreement to the transplant process, referral for transplant eval, getting tons of tests to ensure the individual is an acceptable candidate, finally listing on the waitlist and then… waiting… it’s not like there’s an unlimited supply of kidneys out there. Maybe centers are just referring their healthiest patients, considering the likelihood of getting transplanted is pretty low regardless.
Any of these points might explain the difference between non-profit and for-profit centers. And while the evidence held up to adjustment for some patient factors, case mix may play a role here. In a sensitivity analysis, the authors looked at individuals who SWITCHED from a non-profit to a for-profit center and found their rates of listing and transplant looked pretty much like a standard non-profit patient.
In other words, there’s no doubt more to the story. That said, it’s clear that the financial incentives are misaligned currently, for both for-profit and not-for-profit centers.
In a somewhat encouraging development, Health and Human Services secretary Alex Azar has announced the “Advancing American Kidney Health Initiative” which aims to address some of these incentives – providing new payment models for getting your patients transplanted. The devil is in the details of course, so we’ll all be watching closely to see if the profit motive can be motivated towards transplant.